Generality
Trochanteric bursitis is an inflammatory disease that affects one or more synovial bursa of the proximal femoral epiphysis. It has mainly mechanical (functional or traumatic) causes and causes pain in the affected site, even in association with swelling and redness.
To prevent it from getting worse or chronic, it is important to consult a doctor, who will prescribe drug therapy and physiotherapy; surgery is almost never necessary. The prognosis is generally a few weeks, but the answer is individual.
The prevention of recurrences consists mainly in the possible compensation of functional defects.

What is that
Brief anatomical reference of the trochanter
Large and small trochanter are two bony prominences of the proximal epiphysis of the femur (long thigh bone interposed between the pelvis and the leg).
Both are located at the base of the femoral neck: the large trochanter is located on the lateral face, while the small trochanter is positioned medially and lower.

The muscles interact with the large trochanter: external obturator, small buttock, middle buttock, internal obturator, twins and pear-shaped. The muscles interact with the small trochanter: large psoas and iliac (also known as a single muscle called ileo-psoas).
Meaning of trochanteric bursitis
The trochanteric is the most common bursitis of the coxofemoral area, as well as the most frequent cause of the so-called " painful syndrome of the great trochanter ".
Trochanteric bursitis refers to the inflammation of one, two or all three synovial bags placed above and below the large trochanter (called superficial bag and deep bags).
Normally deflated and small, trochanteric bags are essential for improving tendon flow and for cushioning possible shocks, preserving weak tissues.
The trochanteric bursitis of the superficial bursa (between the great trochanter and the fascia lata) is more frequent, generally not too severe, whereas when the bursitis also involves the deep bursae (between the tendon of the great gluteus and the bone or within the tendon of the small buttock) the clinical picture is often more complicated.
Causes
Risk factors of trochanteric bursitis
Trochanteric bursitis can be triggered by an inflammatory process due to the mechanical action of muscles or tendons, which rub against the bag or push it against the femur.
However, it occurs more often due to a bruise, frequently in correspondence with a fall trauma or heavy contact in certain sports (such as rugby).
Less frequently, it is the result of a modest and continuous, gradual stimulus, such as the repetitive trauma manifested in running (especially in the presence of weak muscles or incomplete technique), uphill walking (even walking) and cycling (especially when the tube of the saddle is badly adjusted, too high).
Trochanteric bursitis can also be a secondary damage caused by chronic conditions such as:
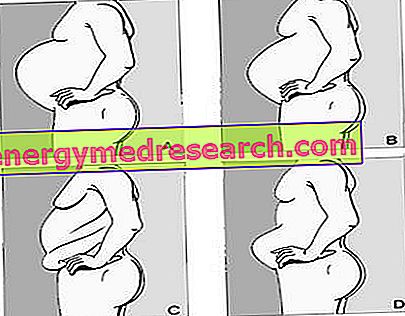
- Scoliosis - lateral curvature of the spine
- Leg length difference
- Weakness of the hip muscles
- Osteoarthritis (degenerative joint disease) of the coxo-femoral or rachis
- Calcifications on tendons of the gluteus maximus muscle flowing over the bag
- Rheumatoid arthritis.
Symptoms and Complications
Symptoms of trochanteric bursitis
The main symptom of trochanteric bursitis is pain - weak or intense, continuous or sometimes limited to certain situations - which increases or decreases depending on posture and movement. In cases of severe trochanteric bursitis, swelling and redness can also be distinguished in the trochanteric area (on the side).
The pain of trochanteric bursitis can manifest itself in different ways:
- Pain and swelling located on the side of the affected side
- Pain that runs through the entire outer thigh and can continue up to the knee
- Pain during sleep; especially when you sleep long on the affected side
- Pain during the act of getting up from a sitting position, especially after long periods (for example when working at a desk or driving), particularly when the coxo-femoral articulation is very closed (eg low chair)
- Pain when climbing stairs
- Cross-legged sitting pain
- Increased pain in walking, cycling or standing if for long periods of time.
When should I go to the doctor?
The perception of pain is sufficient to require the opinion of the doctor. Moreover, especially when swelling and redness also occur, or when the pain seems unjustified and / or becomes limiting, or if the condition resists the GP's treatments (generally consisting of functional discharge and anti-inflammatory drug therapy with oral NSAIDs), it is it is essential to contact a specialist.
Complications
The most frequent complications of trochanteric bursitis are:
- Worsening of the quality of life, with alteration of sleep and difficulty in daily activities
- Overloading of the healthy limb
- Motor impairment and inability to perform certain movements of the thigh and hip
- Thinning and muscle weakness
- Tendency to chronic inflammation.
Diagnosis
Instrumental tests for the diagnosis of trochanteric bursitis
The diagnosis consists primarily of the analysis of symptoms (medical history) and the objective examination. The most characteristic clinical sign, perceptible to palpation, is the softness of the bag.
The doctor can also prescribe instrumental tests (ultrasound or MRI), which will be interpreted by an orthopedist.
It will then be the orthopedist himself or a physiatrist, sometimes in collaboration with a physiotherapist, to determine whether the primary cause of trochanteric bursitis is due to an anatomical or postural complication.
Therapy
Drugs for trochanteric bursitis
As anticipated, the inflammatory state of the trochanteric bursitis can be fought through the use of anti-inflammatory drugs, first NSAIDs orally (mainly ibuprofen) and in case of need also corticosteroids for injection. It is in fact possible to apply a single dose of steroidal active ingredient, together with an anesthetic, directly into the affected bag. Note : this practice should preferably be performed with the ultrasound guide.
Physiotherapy
The physiotherapist is able to perform an evaluation of the clinical history, performing a remote anamnesis and a physical examination of the coxo-femoral joint, the pelvis and the back.
It does not mainly intervene on the regression of the inflammatory state, but it can help reduce pain by applying discharge exercises, massages in the affected area, electrotherapy, etc. It also establishes the need for a brace to walk.
Neuro-motor therapy will be organized to achieve the following goals: restoration of joint movement, muscle length and resting tension, strength and endurance, proprioception, balance and walking.
The last phase is preventive; if necessary, the physiotherapist can decide to strengthen certain muscles by modifying / restoring (depending on the case) the posture and the ability to move, or to apply a plantar to compensate for a shorter limb.
Surgery
Surgery is not a common solution in trochanteric bursitis. However, in the most recurrent and serious cases, one can opt for an arthroscopic removal of the bursa or for a bursectomy.
Tips and home remedies
Trochanteric bursitis is a typically inflammatory disease, therefore the daily application of cold compresses (ice) is of great help to combat both pain and swelling of the tissues.
Prognosis
The prognosis of trochanteric bursitis is not always the same; on the contrary, it varies a lot according to the subjectivity, the conditions of the organism, the triggering causes, the gravity and the type of bursitis.
Some people respond very well to pharmacological and physiotherapy treatment, even within a few weeks; on the contrary, the chronic cases in which a gluteal tendinopathy persists can take many months to obtain a total recovery.
In most cases, trochanteric bursitis heals in about six weeks, during which time pharmacological and physiotherapy (hip muscle control) is adopted. In this period it is essential not to interrupt the physiotherapy activity, not even to the reduction or early disappearance of the pain.
Prevention
Muscle weakness, excessive fatigue and functional overload (or incorrect application of the load) are the main causes of trochanteric bursitis. The best preventive system to avoid relapses consists of a series of measures, which can be summarized as follows:
- Maintain muscle tropism, posture and the correctness of motor patterns
- Wear appropriate footwear, especially in the event of a biomechanical imbalance in the feet
- Manage weight, avoiding overweight and maintaining normal weight
- Technical correction in athletic athletic gesture.