Generality
Eosinophilic esophagitis is a chronic inflammatory disease of the esophagus.

The inflammatory process is supported by an immune-mediated reaction, in which a large number of eosinophils, a particular type of white blood cells, intervene.
The causes of eosinophilic esophagitis are still unknown, but inflammation may depend on the combination of genetic and environmental factors. Often, this condition is associated with allergic syndromes induced by food antigens . Eosinophilic esophagitis can occur in both children and adults, predominantly male.
People suffering from eosinophilic esophagitis most commonly manifest dysphagia, food bolus occlusion, gastroesophageal reflux and retrosternal burning (heartburn). Over time, inflammation of the esophagus can lead to chronic narrowing (stenosis) of the latter.
The diagnosis of eosinophilic esophagitis is based on the endoscopy of the upper digestive tract associated with biopsy of the esophageal mucosa.
In most patients, corticosteroid therapy, elimination of dietary antigens from the diet and possible endoscopic expansion of the esophagus allow good control of symptoms.
What's this
Eosinophilic esophagitis is a chronic condition that can affect the esophageal mucosa at any age.
The inflammation underlying the disorder is immune-mediated (ie caused by the immune system, according to the mechanism of autoimmune diseases).
The symptoms of eosinophilic esophagitis may include: pain or difficulty swallowing (dysphagia), reflux, heartburn and vomiting. In some patients, the esophagus may narrow to the point of blocking the passage of food.
Causes
The exact causes of eosinophilic esophagitis are still not entirely clear. However, the association of inflammation of the esophagus with allergic and / or atopic pathologies is known (in about 70% of cases, eosinophilic esophagitis is concomitant with allergic rhinitis, bronchial asthma or atopic dermatitis).
In people with a genetic predisposition, eosinophilic esophagitis is mainly induced by the ingestion of particular food antigens (eg milk, eggs, soy, etc.), but the reaction can also be triggered by environmental allergens .
Physiopathological mechanisms
Eosinophilic esophagitis is associated with dysfunction of the esophagus resulting from predominantly eosinophilic inflammation.
As regards the maintenance of the inflammatory process, a significant role is played by the overexpression of some mediators (including interleukins and chemokines), which "recall" the eosinophils (through chemotaxis) and regulate their activation. This explains the high density of these immune cells at target tissue levels and the resulting injuries.
Eosinophilic esophagitis: what are eosinophils?
Eosinophilic oesophagitis owes its name to the fact that the disease is characterized by a strong accumulation of eosinophils (also called eosinophilic granulocytes) in the squamous epithelium of the esophagus; these cells are usually involved in immune responses to allergens or parasitic infestations.
In the case of eosinophilic esophagitis, a large number of eosinophils infiltrate the epithelial tissue of the esophagus, causing a variety of gastrointestinal symptoms such as reflux, frequent vomiting, difficulty swallowing and abdominal pain.
Who is most at risk
- Eosinophilic esophagitis can appear at any time, but it occurs mainly in the period between infancy and adulthood . Only on a few occasions does the disease appear for the first time in older people.
- Eosinophilic esophagitis is more common in male subjects. The prevalence in men compared to women is 3: 1.
- Eosinophilic esophagitis is often associated with allergic syndromes. The condition is most likely to occur in people with bronchial asthma and food allergies .
- A greater frequency of eosinophilic esophagitis is observed in patients with close family relationships, supporting the hypothesis of a genetic basis.
Symptoms and Complications
Eosinophilic esophagitis is characterized by alternating periods of remission and activity .
The symptoms of eosinophilic esophagitis vary with age and may include pain or difficulty swallowing (dysphagia), reflux, heartburn and vomiting. In some patients, the esophagus may narrow to the point of obstructing or blocking the passage of the food bolus.
Adults
In adults, the most common presentation symptom of eosinophilic esophagitis is the difficulty in swallowing ( dysphagia ), especially for solid foods.
Less frequently, eosinophilic esophagitis can be associated with other esophageal disorders, similar to those of gastroesophageal reflux disease, such as heartburn, heartburn (retrosternal burning sensation) and chest pain . These latter manifestations do not usually respond to proton pump inhibitor drugs.
Eosinophilic esophagitis can also occur with:
- Retrosternal, epigastric and / or abdominal pain;
- He retched;
- Anorexia and early sense of satiety.
Over time, the inflammation also involves the arrest of the alimentary bolus and the narrowing of the esophageal caliber (or stenosis).
Sometimes, non-esophageal disorders may be present, such as diarrhea, recurrent or chronic laryngitis, recurrent asthmatic crises and bronchopneumonia ab ingestis.
children
During childhood, eosinophilic esophagitis occurs mainly with typical reflux disorders that are not responsive to usual therapy, such as heartburn and food regurgitation .
The inflammation of the esophagus can also be associated with less specific symptoms, such as:
- Vomiting with frequent presence of mucus;
- Inappetence and refusal of food;
- Agitation and crying during the meal;
- Rumination;
- belching;
- Hiccup;
- Abdominal or thoracic pain;
- Intolerance to some foods;
- Reduced weight growth or weight loss;
- Retrosternal burning;
- Epigastric or abdominal pain.
Concurrent complications and pathologies
- Untreated chronic inflammation can lead to narrowing (stenosis) of the esophagus.
- People with eosinophilic esophagitis can have manifestations of allergies or other atopic diseases (such as asthma, allergic rhinitis, eczema, etc.).
Diagnosis
Eosinophilic esophagitis is considered by the doctor when episodic dysphagia, esophageal food obstruction or non-cardiac chest pain occur. The diagnosis is formulated with endoscopy of the upper digestive tract, supported by the biopsy.
Complete clinical history
Generally, the first symptoms appear in young adults (from 20 to 30-35 years), but age at diagnosis can be very variable (1-89 years). The disease can be suspected by the doctor even when the gastro-esophageal reflux does not respond to acid-suppressive therapy with proton pump inhibitors (even at high doses).
Endoscopy of the upper digestive tract
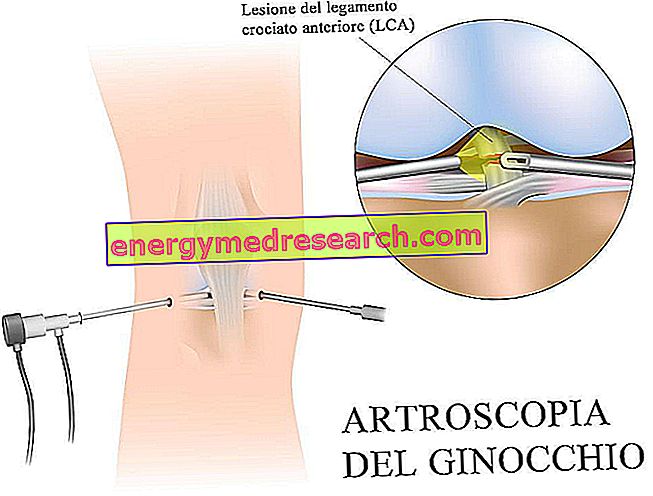
The diagnosis of eosinophilic esophagitis is confirmed after performing an endoscopy of the upper digestive tract with a flexible probe (esophagogastroduodenoscopy, EGDS).
Endoscopic pictures often associated with eosinophilic esophagitis include:
- Longitudinal narrowing of the esophageal gauge or isolated stenosis (proximal or distal);
- Longitudinal discontinuities of the mucosa along the entire course of the esophagus;
- Exudate or diffuse whitish punctuation of the mucosa;
- Widespread nodularity and / or graininess;
- Multiple oesophageal rings, not completely smoothed by insufflation (feline folds or feline feline esophagus);
- Pseudo-diverticulosis.
As the endoscope passes, the esophageal mucosa, due to its frequent fragility, can bleed or crack.
The radiological study with a baritized meal can be indicated as a complementary endoscopy exam. In addition to confirming the reduction in the size of the esophagus, this assessment provides information on the distensibility of the walls.
Biopsy of the esophageal mucosa
During endoscopy, the doctor takes tissue samples for microscopic examination ( biopsy ). Bioptic examination demonstrates the presence of significant eosinophilic infiltration (more than 15 eosinophils / high microscopic magnification field) at the level of the squamous epithelium of the esophagus. Biopsy samples are essential to establish the diagnosis of eosinophilic esophagitis, as the appearance of the esophageal mucosa can be apparently normal to endoscopic vision.
In the patient with associated gastrointestinal disorders (eg diarrhea and abdominal pain), at the bioptic sampling of the esophagus, the removal of tissue from the stomach and duodenum must be added; this allows to verify the involvement of eosinophilic infiltration and to exclude other concomitant pathologies.
Number of eosinophils and differential diagnosis
The presence of the eosinophilic infiltrate in the squamous epithelium of the esophagus is common to several pathological conditions, including: gastro-oesophageal reflux disease, parasitosis, Crohn's disease and lymphoma . The "discriminating" element is quantity: in eosinophilic esophagitis, eosinophils are numerically higher than these conditions.
For this reason, it is essential that the anatomopathologist quantifies the density of eosinophils by microscopic field. Conventionally, in order to diagnose eosinophilic esophagitis, it is necessary to find a number equal to or greater than 15 eosinophils for HPF (high power field, ie x400 magnifications), in association with other features of the eosinophilic infiltrate.
Test for allergies
In order to identify the possible factors involved in eosinophilic oesophagitis, the doctor can subject the patient to tests for food and respiratory allergies, possibly associated with skin tests (Prick test) or radioallergosorbent test (RAST).
In summary: diagnostic criteria of eosinophilic esophagitis
The criteria for establishing the diagnosis of eosinophilic esophagitis are:
- Presence of esophageal symptoms (dysphagia, alimentary bolus occlusion, heartburn and reflux);
- ≥ 15 eosinophils / HPF at histological analysis of the biopsy sample;
- Absence of clinical response to full-dose proton pump inhibitors .
Treatment
The possibilities for treating eosinophilic esophagitis include various interventions. In most cases, topical corticosteroid therapy, elimination of dietary antigens from the diet and possible endoscopic dilation allow good control of symptoms.
Dietary changes
- If the allergy to a food is strongly suspected based on the patient's clinical history and is found with objective allergy tests, the doctor may indicate a targeted elimination diet .
- In the absence of specific sensitization to foods, the diet of the patient with eosinophilic esophagitis may include the empirical elimination of the main allergens (milk, egg, wheat, soy, peanuts and fish), indicatively for 8-12 weeks.
- In patients with multiple allergies, however, the doctor may prescribe an elemental (amino acid) diet, with the exclusion of all whole proteins.
The decision to use a specific dietary approach is more effective in children than in adults.
Management of eosinophilic esophagitis in infancy
In children, the initial therapy of eosinophilic esophagitis can:
- Be the deprivation diet based on specific allergy tests;
- Predict the elimination of the most common allergenic foods .
In general, the results of this intervention are satisfactory and, in many cases, limit the need for corticosteroid therapy.
Topical corticosteroids
The most useful drugs for controlling the symptoms of topical esophagitis are topical corticosteroids (such as fluticasone propionate and budesonide ).
The route of administration with a multi-dose oral inhaler is the preferred one (in consideration of the absence of side effects secondary to systemic therapy and of the high topical anti-inflammatory efficacy). In case of eosinophilic esophagitis, it is possible to nebulize the drug in the mouth and swallow it: in this way, the drug coats the esophagus and does not penetrate the lungs. Alternatively, budesonide can be mixed with a sugar substitute before being swallowed.
After taking the patient, the patient must rinse the oral cavity with water (to avoid a fungal infection, such as candidiasis) and do not drink or eat for at least 30 minutes (to maximize topical anti-inflammatory action at the level of the esophageal mucosa ).
Topical corticosterodes for the treatment of eosinophilic esophagitis are usually given for 6-8 weeks, 30 minutes before breakfast and 30 minutes before dinner. This therapy is to be repeated when symptoms recur.
Endoscopic therapy
- When subjects have recurrent episodes of dysphagia and have a significant stenosis, the doctor can intervene using a hydrostatic balloon or a solid esophageal dilator . Esophageal endoscopic dilation is performed by experienced endoscopists with extreme caution, to prevent esophageal lacerations or perforations.
- In the case of an alimentary bolus occlusion, the endoscopic dilation allows the rapid dissection of the esophagus.
Prognosis
The complications of untreated eosinophilic esophagitis include fibrosis of the lamina propria and the formation of narrowings that increase the risk of food obstruction and perforation of the esophagus .
The correct management of the pathology allows the patient to maintain a good quality of life.