Generality
Type 2 diabetes is the most common form of diabetes mellitus, a metabolic disorder characterized by hyperglycemia.
At the origin of type two diabetes there are generally 2 alterations: insulin resistance and a deficiency of secretion of the hormone insulin, by pancreatic cells responsible for this function.

In type 2 diabetes, the goal of therapy is to bring the blood sugar back to normal levels.
To achieve the aforementioned goal, the indispensable treatments are: a healthy and balanced diet, and the regular practice of physical exercise.
Brief review of diabetes mellitus: what is it?
Diabetes mellitus, or more simply diabetes, is a metabolic disease whose onset is linked to insulin, a key hormone for maintaining normal blood glucose levels.
There are different types of diabetes mellitus, some decidedly more common and known than others. The most common types include type 1 diabetes, type 2 diabetes and gestational diabetes; among the less common, however, are the so-called secondary diabetes and MODY diabetes.
The characteristic that all types of diabetes mellitus have in common is hyperglycemia, which is the high concentration of glucose in the blood.
To learn more: Types of Diabetes
What is type 2 diabetes?
Type 2 diabetes is a type of diabetes mellitus in which hyperglycemia can depend on two alterations:
- The unusual resistance of tissues to the action of insulin ( insulin resistance )
- The progressive and relentless decline in the capacity of the Langerhans islands to produce insulin (insulin secretion deficiency ).
These two alterations can act individually or, as happens in most circumstances, they tend to add up to one another.
Epidemiology
Type 2 diabetes is the most common form of diabetes mellitus ; according to the most reliable estimates, in fact, about 90% of diabetics present around the world would be carriers of it (NB: the restante 10% of diabetes cases are mainly type 1 diabetes and gestational diabetes).
Type 2 diabetes most often affects adults; in particular, the latter tendency to develop the metabolic disease in question becomes progressively more consistent starting from 35-40 years. The rate of onset of type 2 diabetes in young subjects is quite modest, although, in recent years, it has recorded a significant increase compared to several decades ago.
Type 2 diabetes is closely associated with the problem of obesity, which is probably one of the most important risk factors.
In the last 30 years, the worldwide spread of type 2 diabetes has increased almost exponentially: if in 1985 the diagnoses of type 2 diabetes were about 30 million, in 2015 they reached 392 million.
Causes
According to doctors and scientists, type 2 diabetes would depend on a combination of genetic factors, which give a certain predisposition to the development of the disease in question, and environmental factors, which act as concretizing elements of the aforementioned predisposition.
What are the most important environmental factors?
Among the most important environmental factors, as regards the development of type 2 diabetes mellitus, are:
- Obesity . The increase in body weight leads to an increase in the synthesis of triglycerides, which, being in excess, also accumulate in pancreatic cells. The accumulation of triglycerides in pancreatic cells decreases the function of the latter;
- A sedentary lifestyle . In contrast, physical exercise hinders the onset of type 2 diabetes;
- Aging . Advanced age seems to contribute to the manifestation of genetic defects that are the basis of type 2 diabetes;
- A diet rich in simple sugars . Absorption of simple sugars requires a lot of insulin. Therefore, in a person predisposed to type 2 diabetes mellitus, taking too many simple sugars has the effect of exhausting the already limited capacity for genetic reasons of the pancreatic beta cells to produce insulin.
- Hypertension ;
- HDL cholesterol levels (the so-called "good cholesterol") less than or equal to 35 mg / ml;
- Triglyceride levels greater than or equal to 250 mg / ml.
Outline of physiopathology
Typically, type 2 diabetes begins with tissue resistance to insulin action (insulin resistance).
Insulin resistance, therefore, gives rise to a greater demand for insulin, a demand that, however, the beta cells of the Langerhans islands are unable to fulfill properly.
The need for more insulin, combined with the difficulty of pancreatic beta cells in satisfying the aforementioned need, is responsible for an increase in blood sugar beyond the norm and a worsening of functional capabilities - already partially compromised for a genetic predisposition - of the beta cells themselves pancreatic; on the latter, in fact, it is as if the demand for more insulin had the effect of accelerating the decline to which they have always been destined.
Type 2 diabetes risk factors
Briefly, the risk factors for type 2 diabetes are:
- Overweight and obesity;
- A sedentary lifestyle;
- A family history of type 2 diabetes;
- Belonging to the black, Hispanic, Indian or American American race;
- Advanced age;
- A past history of gestational diabetes;
- The polycystic ovary;
- Hypertension;
- High triglyceride levels and low HDL cholesterol levels.
Symptoms, signs and complications
Dependent on the presence of hyperglycemia, the typical symptoms of type 2 diabetes consist of:
- Polyuria, ie need to urinate often;
- Polydipsia, that is an intense sense of thirst;
- Polyphagia, that is strong appetite;
- Recurrent asthenia (fatigue);
- Blurred vision;
- Slow healing from wounds.
Sometimes, to these symptoms, others may be added, including:
- Headache;
- Skin itching;
- Irritability;
- Ease of developing infections.
How do you start?
Unlike type 1 diabetes, which begins fairly quickly, type 2 diabetes is established very slowly and takes a long time (even years) to manifest symptoms related to hyperglycemia; in some patients, it may even happen that these symptoms always remain very mild, almost imperceptible.
The slow appearance and above all the tendency of the symptomatology to remain mildly explain why, quite frequently, the diagnosis of type 2 diabetes occurs by chance, during laboratory tests performed for other reasons.
A metabolic state intermediate between normality and type 2 diabetes: prediabetes
Quite frequently, people with type 2 diabetes have previously suffered from prediabetes, a metabolic condition that lies between normal and true diabetes mellitus (type 2).
Existing in two forms, known as impaired fasting glucose and impaired glucose tolerance, prediabetes are almost always symptom-free and are reported for only one alteration, certainly important, which is hyperglycemia.
Most relevant clinical signs
The characteristic clinical signs of type 2 diabetes that classically emerge from blood and laboratory tests are, in order of importance:
- Fasting and post-meal hyperglycemia;
- Glycosuria;
- Hypertriglyceridemia (or high triglycerides);
- Hyperuricemia (increase in the amount of uric acid in the blood).
Remembering that often the patient with type 2 diabetes is an obese person, faced with the concomitant presence of fasting hyperglycemia, high triglycerides, hyperuricemia and obesity, doctors talk about a condition known as metabolic syndrome .
Complications
Type 2 diabetes is a disease from which, with some ease, complications can arise, some even very serious and with potentially lethal effects.
Very probably dependent on hyperglycemia, the complications of type 2 diabetes are distinguishable in acute and long-term (or chronic).
The acute complications can be summarized, substantially, in the so-called non-ketosic hyperosmolar coma, a clinically very relevant condition that can lead first to unconsciousness and then even to death.
To learn more: Acute Complications of Diabetes
Long-term complications, on the other hand, consist of alterations affecting large arterial blood vessels ( diabetic macroangiopathy ) and capillaries ( diabetic microangiopathy ), which gives rise to a greater tendency to develop cardiovascular diseases and pathologies such as diabetic nephropathy, retinopathy diabetic, diabetic ulcer (see diabetic foot), diabetic neuropathy, cataract, etc.
To learn more: Long-term complications of diabetes
When should I go to the doctor?
The presence in an adult individual of the need to urinate often, associated with intense sects and risk factors typical of type 2 diabetes (eg, obesity, hypertension, sedentary lifestyle and high triglycerides), represents an important alarm bell and deserves a immediate medical consultation.
Diagnosis
As stated, a feature always present in type 2 diabetes (and in all forms of diabetes mellitus) is hyperglycemia; therefore, the verification of the latter is fundamental in the diagnosis.
To determine the presence of hyperglycemia, a venous blood sample is taken and the subsequent measurement, on this venous blood just taken, of the amount of glucose present.
According to the latest criteria proposed by the experts of the ADA ( American Diabetes Association ), a person suffers from diabetes when the following three conditions are met:
- Blood glucose (ie blood glucose concentration) is> 200 milligrams of glucose per deciliter of blood (mg / dl) at any time of the day.
- Fasting blood sugar is> 126 mg / dl.
In normal conditions it should be less than 100 mg / dl.
- The blood sugar level after 120 minutes from the OGTT (oral glucose tolerance test or oral glucose load test) is> 200 mg / dl.
In normal conditions it should be less than 140 mg / dl.
How to distinguish type 2 diabetes from type 1 diabetes
In almost all circumstances, doctors are able to distinguish type 2 diabetes from type 1 diabetes through physical examination, analysis of the patient's medical history and other characteristics of the latter such as age. .
If despite these assessments doubts remain, the tests that allow us to eliminate all doubts are two:
- An antibody test specific for type 1 diabetes. It should be noted that type 1 diabetes is an autoimmune disease, which presents abnormal levels of some particular antibodies.
- The quantification of the levels of peptide C, a fundamental constituent of the insulin precursor, which in the case of type 2 diabetes is normal or high, whereas in the case of type 1 diabetes it is less than normal.
| Table. Elements that make it possible to distinguish type 2 diabetes from type 1 diabetes, without the need for extensive tests. | |
| Typical elements of type 2 diabetes | Typical elements of type 1 diabetes |
Appearance in adulthood; Presence of risk factors, such as obesity, sedentary lifestyle, polycystic ovary, high triglycerides associated with low levels of HDL and hypertension; Family history of type 2 diabetes; Belonging to the black, Hispanic, Indian or American American race; Slow onset of symptoms and not always marked symptoms. | Appearance in youth; Family history of type 1 diabetes; Quite fast onset of symptoms and marked symptoms. |
Therapy
Type 2 diabetes is a chronic disease from which it is impossible to heal, but which, with adequate treatments, is largely controllable.
Like all other types of diabetes, even in the case of type 2 diabetes, the treatment has the ultimate goal of bringing back too high levels of blood glucose. Moreover, symptoms and complications of type 2 diabetes (and all other types of diabetes) depend on hyperglycemia.

Finally, the last aspect to be reported, in this overview concerning the treatment of type 2 diabetes, is the periodic control of the effects of the ongoing therapy . With a generally weekly frequency (at least in the first period of the illness), this check is useful to the attending physician to understand if the adopted treatments are working or if they need a modification, because ineffective or scarcely effective.
| Table. The treatment of type 2 diabetes in brief. | |
| Therapeutic purpose | Bring excessively high blood glucose levels back to normal |
Pivotal treatments | Healthy and balanced diet Regular exercise |
Complementary care | Pharmacological therapy based on oral hypoglycemic agents (NB: if they have lost their effectiveness, synthetic insulin is used) |
Blood glucose control | Weekly, especially in the early stages of the disease |
To know more:
- Diabetes Care
- Hypoglycemic crisis
Why is diet important?
In humans, blood sugar is strictly dependent on the food ingested. For example, a high-sugar meal results in a marked rise in blood sugar (as well as an abundant production of insulin).
In light of this, it is easy to understand the importance that a certain type of diet has on the control of an altered blood glucose, such as that present in case of type 2 diabetes.
To learn more about type 2 diabetes and diet:
- Example Diet for Type 2 Diabetes
Why is physical exercise important?
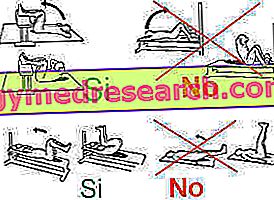
Exercise is useful for type 2 diabetics, because:
- Promotes the passage of glucose from the blood to tissues (especially muscle) through a mechanism independent of insulin. This clearly leads to a reduction in blood glucose levels.
- Improves tissue sensitivity to insulin, counteracting the phenomenon of insulin resistance, which hinders the entry of glucose into cells (and increases the demand for insulin).
Furthermore, physical exercise is important, as it reduces the cardiovascular risk, helps to normalize body weight in cases of type 2 diabetes associated with obesity and, finally, has favorable psychological effects.
To learn more about type 2 diabetes and physical activity:
- Physical Activity and Type 2 Diabetes
- Sports Effects on Type 2 Diabetes