Generality
Depending on the sources consulted, one speaks of fetal macrosomia when the birth weight is greater than 4 kg or 4 kg and a half.
More correctly, the fetal weight should be related not so much to absolute values as to the standards considered normal for its development; hence, in this perspective, any fetus with a weight greater than the 90th percentile of reference for gestational age is defined as macrosomic.
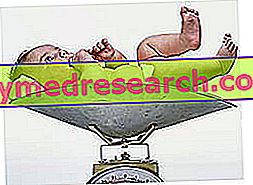
It must be said, however, that before birth the estimate of fetal body weight, performed mainly by ultrasound (ultrasound), is quite inaccurate.
Causes
Approximately eight out of a hundred non-diabetic newborn mothers are macrosomic; in the diabetic population, on the other hand, the incidence rises to 26%. Diabetes, in fact, represents the main risk factor for neonatal macrosomia, regardless of whether it occurs before or during gestation (gestational diabetes). Hyperglycemia and especially hyperinsulinemia represent an important element in stimulating fetal growth. The newborn is so macrosomic, with organomegaly characterized by larger and more numerous cells than those of normal-weight infants.
Other important risk factors for macrosomia include obesity, excessive weight gain during pregnancy, multiparity, a previous pregnancy with fetal macrosomia (the condition can still occur even if it has not occurred in previous gestations), ethnicity (the incidence of macrosomia is higher in the black race), familiarity (it is more probable that a macrosomic child is born when the family members are tall and robust) and duration of the pregnancy (when it lasts over 40 weeks the risk increases of fetal macrosomia). Furthermore, male infants tend to have a higher weight than females.
Risks for the newborn
In most cases, a macrosomic newborn is healthy and in good health. The unborn child can present serious complications if diabetes occurs before pregnancy and is not adequately controlled. On the contrary, when diabetes arises during gestation (gestational diabetes) - by virtue of the fact that it appears when the development of organs and systems is now complete - it does not cause congenital malformations. It is clear that even a diabetic woman can carry out a pregnancy with serenity and without any complication, but it is essential that the conception is preceded by a preventive medical consultation and an optimal control of diabetes before, during and after pregnancy. The conception and the very first weeks of gestation, in particular, must take place in a situation of perfect glycemic control.
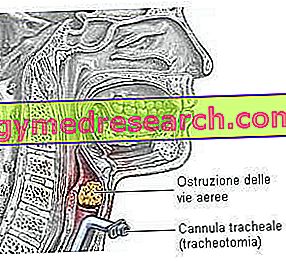
At the time of birth, for obvious reasons, a macrosomal newborn finds it more difficult to come to light naturally, requiring in many cases the use of cesarean section. In the case of natural childbirth, therefore, the risks of vaginal laceration (up to the involvement of the anal sphincter) and post-partum hemorrhages increase for the mother, while the unborn child runs a greater risk of fracture and shoulder dystocia. Furthermore, at the time of birth, the unborn child can suffer a hypoglycemic crisis, since - being used to living in a hyperglycemic environment - it can be affected by the sudden decrease in sugars when the umbilical cord is detached. Other possible complications at birth are represented by hyperbilirubinemia and respiratory distress syndrome.
Macrosomia, like the opposite condition, seems to increase the risk of obesity and its late complications (type II diabetes, atherosclerosis, hypertension) in childhood and in the following age groups.
Prevention
To prevent macrosomia in diabetic women, an appropriate pre-conception consultation is associated with optimal diabetes control before, during and after pregnancy; the expectant mother, on her part, must strictly follow the advice given by the pediatrician and the diabetological team, which includes doctors, nurses, nutritionists and social workers.
As for euglycemic women, however, it is very important to prevent the onset of diabetes during the gestational period. This very important work of prevention is carried out first of all by regularly comparing with the gynecologist and the other assistants. The fundamental recommendations are those of forgetting the old saying "in pregnancy it is necessary to eat for two" and the increasingly widespread tendency to put purely aesthetic concerns before one's own well-being and that of the unborn child. Compliance with the advice on nutrition and the right amount of momentum is essential for the prevention of neonatal macrosomia. A correct dietary - behavioral approach makes it possible to maintain blood glucose levels and body weight within the limits considered "optimal" for pregnancy. If the blood sugar levels are still high, small doses of insulin can be prescribed with meals.