Generality
Colostomy is a somewhat delicate surgical procedure, through which the large intestine is deviated and connected to an opening created specifically in the abdominal wall.
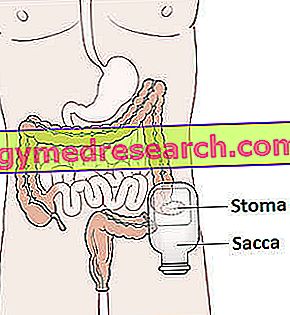
Scheme of a permanent colostomy. Image taken from: //en.wikipedia.org/wiki/Colostomy
Once the connection has been made, this opening (which is more correctly called the stoma) replaces the natural anus, therefore - given the position - it must be equipped with a bag for collecting the faeces.
The bag must obviously be changed and cleaned periodically.
To make a colostomy necessary are several morbid states, such as colorectal cancer or intestinal obstruction.
There are two surgical techniques with which to perform a colostomy: the traditional surgery technique and laparoscopy.
Furthermore, the deviation of the intestine and the stoma can be achieved in different ways, depending on the pathological conditions that require the colostomy.
Short reference to intestinal anatomy. Where is the colon located?
The intestine is the portion of the digestive system between the pylorus and the anal orifice. From the anatomical point of view, it is divided into two main sectors: the small intestine, also called small intestine, and the large intestine, also called large intestine .
The small intestine is the first section; it starts at the level of the pyloric valve, which separates it from the stomach, and ends at the level of the ileocecal valve, located on the border of the large intestine.
The small intestine consists of three sections (the duodenum, the fast and the ileum), is about 7 meters long and has an average diameter of 4 centimeters.
The large intestine is the terminal tract of the intestine and of the digestive system. It starts from the ileocecal valve and ends at the anus; consists of 6 sections (cecum, ascending colon, transverse colon, descending colon, sigma and rectum), is about 2 meters long and has an average diameter of 7 centimeters (hence the name of large intestine).
What is colostomy?
The colostomy is a surgical procedure that involves the deviation of the large intestine (generally of the colon ) towards an opening made on the abdomen. This opening (or stoma ), made to connect to a special waterproof bag, is used to allow faeces to escape.
In other words, the colostomy is the surgery with which the normal intestinal path is modified and an orifice is created on the abdomen, which actually replaces the functions of the anus.
IS IT A TEMPORARY OR PERMANENT REMEDY?
Colostomy may be a temporary (or reversible ) or permanent (or final ) solution to stool removal. In the case of a temporary solution, another surgical operation is foreseen by which the patient's intestine is again placed in communication with the anus.
Statistical data
According to an Anglo-Saxon survey, in the United Kingdom, the annual number of permanent colostomies performed is around 6400.
COLOSTOMY AND OPENING SEAT
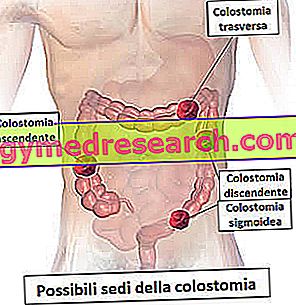
Illustration depicting various types of colostomy. Image taken from: //en.wikipedia.org/wiki/Colostomy
Depending on the tract of large intestine that the surgeon deviates towards the abdomen, the colostomy can also be referred to as:
- Cecostomy, if the cecum is affected
- Colostomy on the ascendant, if the ascending colon is affected
- Colostomy on the transverse, if the transverse colon is affected
- Colostomy on the descendant, if the descending colon is affected
- Sigmoid colostomy, if sigma is affected
When you run
Colostomy is practiced in the presence of certain diseases of the large intestine.
These diseases - which in some cases also require the removal of portions of the colon ( colectomy ) - consist of:
- Colorectal cancer . Colorectal cancer (or colorectal cancer) is the most frequent malignant neoplasm of the gastrointestinal tract and represents a major cause of death from cancer, both in men and women. From the therapeutic point of view, the main treatment is the colectomy operation, through which the affected intestine region is removed. The more the malignant tumor is in an advanced and extended phase, the larger the intestinal tract will be removed.
Sometimes, colectomy for colorectal cancer can end with a colostomy. The latter may be a temporary solution, if the re-joining of the various sections of intestine left (reversible colostomy), or a definitive solution, if the surgeon has also removed the entire rectum (proctocolectomy) is expected.
- Diverticulitis . Diverticulitis is the inflammation of diverticula; diverticula are small extroflections that can form inside the entire alimentary canal, particularly in the colon.
Diverticulitis usually requires drug therapy and the adoption of a healthy diet appropriate to the circumstances. If these treatments are found to be ineffective or late, colectomy may be necessary followed by a colostomy. In these situations, the colostomy is usually temporary, because it is expected to rejoin the various sections of intestine left.
- Crohn's disease . It is an autoimmune disease, belonging to the category of so-called inflammatory bowel diseases. Patients with Crohn's disease can benefit from colostomy in two situations: either after a colectomy or to isolate the inflamed intestinal area from the stool. In the first case, the colostomy could also be permanent (NB: especially if there were precancerous cells in the removed colon); in the second case, instead, it is usually temporary (NB: the return to normality occurs when the inflammation has been reduced at the level of the isolated intestinal portion).
- Bowel obstruction . We talk about intestinal obstruction when the intestine is blocked and does not allow what is flowing inside to progress regularly. Intestinal obstruction is considered a medical emergency, as, where blockage occurs, bleeding, infection and intestinal perforation may occur. Treatment generally involves a colectomy (partial or total, depending on the severity of the occlusion), followed by a colostomy. The temporary nature or permanence of the latter depends on the size of the large intestine removed.
- Fecal incontinence . Those suffering from fecal incontinence are subject to involuntary and uncontrolled leaks of feces and intestinal gas.
The use of colostomy for the treatment of faecal incontinence occurs only when all possible non-surgical treatments have been ineffective.
- Intestinal injury from abdominal trauma . The traumas to the abdomen that can provoke an intestinal injury are: a stabbing, a gunshot wound, an accident in the workplace, a car accident, etc. These wounds to the intestine may require a partial colectomy, followed by a temporary or, in some cases, even permanent colostomy.
- Hirschsprung disease . Hirschsprung's disease is a rare congenital disease that affects one child every 5, 000. Those suffering from it lack some nerve endings that control the colon muscles, therefore it is easily subject to episodes of intestinal obstruction.
The colostomy (temporary or permanent, depending on the severity) is practiced to isolate the non-innervated intestine tract and at risk of occlusion, and to allow the regular stool to escape.

Colostomy bag. From the site: www.berktree.com
Preparation
Colostomy is a procedure that requires general anesthesia . Therefore, before its execution, the individual must be subjected to the following clinical controls:
- Accurate physical examination
- Complete blood analysis
- Electrocardiogram
- Evaluation of clinical history (diseases suffered in the past, possible allergies to anesthetic drugs, medicines taken at the time of checks, etc.).
If there are no contraindications of any kind, the operating surgeon (or a member of his staff) will explain the methods of intervention, the possible risks, the pre- and post-operative recommendations and, finally, the recovery times.
The main pre- and post-operative recommendations:
- Before colostomy, suspend any treatment based on antiplatelet agents (aspirin), anticoagulants (warfarin) and anti-inflammatory drugs (NSAIDs), because these drugs, by reducing the coagulation capacity of the blood, predispose to severe bleeding.
- On the day of the procedure, appear at full fast from at least the previous evening and with the intestine empty and possibly clean . To empty the intestine, the doctor generally recommends a laxative solution to be taken several hours before the operation, while antibiotics are used to clean the intestine.
- After the surgery, be assisted by a trusted person .
EMERGENCY COLOSTOMY
Emergency cases, such as bowel obstruction, require immediate colostomy (and before colectomy) surgery. This prevents, therefore, from scrupulously observing some of the pre-operative recommendations mentioned above (fasting, bowel cleansing, etc.).
Procedure
The surgeon can perform the colostomy operation using one of the following two alternative surgical techniques: the so-called traditional technique (also called " open-air ") and laparoscopy (or laparoscopic technique ).
BEFORE STARTING
Before starting the operation, the patient is anesthetized (NB: an anesthesiologist is involved in this) and connected to various devices that will measure, for the duration of the operation, his vital parameters (blood pressure, heart rate, oxygenation of the blood etc).
TRADITIONAL INTERVENTION
During the traditional colostomy the surgeon makes an incision of several centimeters on the abdomen and, through the resulting opening, carries out the intended intestinal deviation.
Then, once the intestine is connected to the abdominal stoma, it closes the incision and applies stitches.
The traditional colostomy operation is particularly invasive, but guarantees precision and allows curing conditions, such as intestinal obstruction, for which the laparoscopic technique is inadequate.
INTERVENTION IN LAPAROSCOPIA
During laparoscopic colostomy the surgeon performs, at various points of the abdomen, several incisions of about one centimeter, through which he introduces the surgical instrumentation (laparoscope, scalpel, etc.) necessary for the realization of the abdominal stoma and intestinal deviation.
The laparoscopic colostomy procedure is characterized, like all laparoscopic operations, by the minimal invasiveness and the rapidity with which the operative wounds heal. Therefore, except in special cases where use is contraindicated, it represents the most practiced operative technique.
TYPES OF COLOSTOMY
There are at least three different ways to practice intestinal deviation and abdominal stoma. Based on the adopted method, the colostomy is distinguished in:
- Colostomy ad ansa (English, loop colostomy )
- Terminal colostomy, or preternatural anus (English, end colostomy )
- Colostomy with separate orifice, or colostomy "in the discontinuity"
The most commonly used types of colostomy are the first and the second.
COLOSTOMIA AT ANSA: WHAT IS IT?
During a loop colostomy, the surgeon drags a loop of the large intestine out of the future stoma and fixes it to the latter, via stitches. Then, at the end of these operations, it cuts the protruding portion of intestinal loop and joins, on their inner side, the two stumps of intestine that open on the abdominal wall. In this way, two distinct stomata are created, one that comes from the overlying gastrointestinal tract and from which the faeces (proximal canal) and another that starts from the stoma and ends with the anus and from which only mucus (distal canal ).
Immediately after surgery, the region of the stoma is inflamed and particularly swollen. Over the weeks, however, the situation gradually improves and the abdominal opening reaches the desired size. Generally, it takes 8 weeks for swelling and inflammation to resolve completely.
The contours of the stoma lack nerve endings - so, when touched, they do not cause any kind of pain - and tend to bleed easily. Blood losses are minimal and, unless complicated cases, do not represent a problem.
Sometimes, to keep the intestinal loop in place while healing, the surgeon could apply a special instrument, called a stick or bridge, to the stoma.
The loop colostomy usually has temporary purposes and is particularly suitable for cases of diverticulitis, Crohn's disease and colorectal cancer.
TERMINAL COLOSTOMY: WHAT DOES IT WORK?
In fact, the operation of terminal colostomy consists in the creation of an artificial anus, located at the abdominal level. In fact, the surgeon dissects the intestine before where the diseased area resides and puts the healthy stump - which comes from the overlying gastrointestinal tract - into communication with the abdominal stoma.
At the level of the stoma, it shapes the edges of the intestinal tract with the contours of the opening on the abdomen and applies the sutures that serve to block the deviation.
The intestine stump connected to the natural anus (and insulated because it is sick) can undergo two different fates:
- If there are no possibilities for its recovery (for example in the case of cancer), it is removed (colectomy).
- If an improvement in his condition is possible, he is left in place for a possible restoration of a normal gastrointestinal canal.
The terminal colostomy has, in general, permanent purposes and is particularly appropriate for cases of intestinal obstruction, traumatic lesion and colorectal cancer.
COLOSTOMIA A SEPARATE ORIFICE
The colostomy with a separate orifice is performed in a completely analogous way to the colostomy with a loop, with the only difference being that the two channels, at the level of the stoma, are separated by a flap of skin appropriately sutured by the surgeon. Thus, while in the colostomy with loop the two abutments are adjacent to each other, in the colostomy with separate orifice they are divided.
The space that divides the two channels is really thin, so much so that we talk about a stoma only.
Post-operative phase
At the end of the colostomy, there is a hospitalization that can last from a minimum of 3 to a maximum of 10 days. The duration generally depends on the severity of the intestinal problem that made the colostomy operation necessary.
Usually, in the first days after the operation, the patient is fed intravenously and subjected to bladder catheterization (for the elimination of urine).
The stool collection bag is obviously applied immediately: initially and until the inflammation of the stoma has been reduced, the doctors use a large and uncomfortable one; then, as the swelling at the level of the abdominal opening is reduced, they resort to a small one.
MANAGEMENT OF THE BAG AND HYGIENE OF THE STOMA
During admission, a member of the medical staff teaches the patient how to take care of the bag (when to change it, when to understand that it is full, etc.) and how to keep the stoma and the surrounding area clean.
Proper management of the stool pouch and careful cleaning of the stoma reduce the risk of infection.
FIRST DAYS AFTER THE RESIGNATION
For the first time, after discharge, it is good that the patient avoids carrying out heavy activities (lifting weights, etc.); these, in fact, could affect the recovery and the success of the intervention.
Furthermore, until the intestinal surgical wounds have healed completely, it is likely that an unpleasant odor will come out of the stoma.
LACK OF BURST
Unlike the natural anus, the abdominal stoma lacks sphincters, therefore the leakage of feces and air is completely uncontrolled. This could cause some embarrassment, especially in the beginning.
Risks and complications
As during any surgery, even during the execution of a colostomy there is a risk of:
- Internal bleeding
- Infections
- Formation of blood clots in the veins
- Stroke or heart attack during the operation
- Allergic reaction to anesthetic drugs or sedatives used during surgery
Furthermore, once the operation is completed and due to the extreme delicacy of the intervention, a series of different complications can occur, such as:
- Loss of mucus from the portion of rectum remained . If rectum and sigma are not removed, it is likely that, although isolated from the rest of the intestine, they still produce mucus and disperse it through the anus. In these cases, the patient is forced to go to the toilet from time to time to clean up small leaks.
- Skin irritation due to mucus loss . Sometimes mucus leaks can irritate the skin surrounding the anus. In these situations, it is advisable to use spreadable creams, specifically designed to reduce skin irritation.
- Parastomal hernia . We speak of a parastomal hernia when a tract of intestine, located near the stoma, wedges itself through the surrounding muscular wall and gives rise to a swelling.
- Stoma occlusion . The stoma may become blocked due to an accumulation of food inside the intestine; in such circumstances, the typical symptoms are: nausea, vomiting, abdominal cramps, stoma enlargement, reduced stool production, etc. If after two hours the stomal occlusion does not improve, it is good for the patient to contact his doctor and ask him for advice on what to do.
- Skin problems . The skin around the stoma may become irritated and inflamed. If irritation and inflammation are particularly painful, contact your doctor.
- Stomal fistula . The stomal fistulas are small channels that form next to the stoma and that connect the latter with the skin. Their appearance requires the adoption of a suitable stool collection bag.
- Stomach prolapse . One speaks of stomal prolapse when there is a protrusion of the intestinal tract that constitutes the stoma. If the stomal prolapse is mild, it is sufficient to use a collection bag for ad hoc faeces; if, instead, the prolapse of the stoma is marked, it is necessary to intervene surgically.
- Stoma stenosis . The term stenosis means narrowing, so the stomal stenosis is the narrowing of the stoma. To cause a stomal stenosis is the formation of scar tissue in correspondence of the opening that allows the passage of the feces. In the case of stomal stenosis, a second colostomy operation is needed.
- Stoma retraction . There is stomal retraction when the portion of intestine that constitutes the stoma retracts slightly backwards making it difficult to apply the bag for stool collection. If the stomal retraction is severe, surgery is needed.
- Internal or external leaks . At the points where the intestine is sealed (both at the stoma level and internally), faecal contents may leak. Especially internal leaks require corrective surgery.
- Stoma ischemia . Stoma ischemia occurs when the blood supply to the stoma is reduced or completely missing. Failure to take corrective action could lead to necrosis of the affected intestinal tissue.
Colostomy and daily life
Although it imposes some limitations, colostomy still allows one to lead an active and social life.
The greatest attention should be paid to the diet (especially in the first phase of post-operative recovery) and to the periodic change and cleaning of the bag for stool collection.
Regarding work, exercise and sexual intercourse, it is advisable to seek advice from your doctor or the surgeon who performed the colostomy. In fact, each patient represents a case in itself.