Generality
Pyelonephritis is an acute or chronic inflammatory disease of the kidney and renal pelvis, usually accompanied by an infection of the parenchymal tissue of the organ. The symptomatology of the disease is characterized by fever, lower back pain and symptoms in the lower urinary tract.
Causes
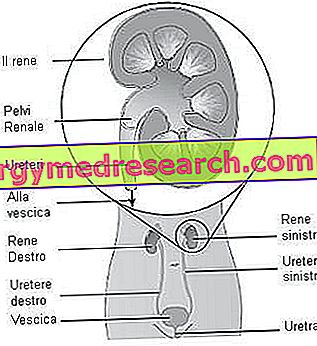
The origin of pyelonephritis is bacterial and the ways in which the infection spreads can be different. The colonization mediated by pathogens can in fact take place through:
- Ascending pathway from the bladder (the most frequent): from the perineum (or from the vaginal vestibule, in the case of female patients), the microorganisms go back up into the urethra, then into the bladder, up to the kidney; the main causes of infection for women consist in deformation of the urethra during sexual intercourse, while for men it is often secondary to prostatitis.
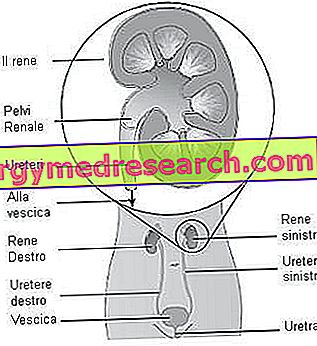
- Descending blood pathway: through the bloodstream, during septicemia, pathogens reach the kidney causing renal nephritis and abscesses.
- Lymphatic descending pathway: a network of lymphatic vessels connects the ascending colon with the right kidney and the descending colon with the left kidney.
The microorganisms involved in pyelonephritis are usually the same as those responsible for infections of the urinary tract, genital and gastro-enteric apparatus, and therefore in the bladder, prostate, cervix, vagina, urethra or rectum: Escherichia coli, Klebsiella spp., Proteus spp ., Enterococcus spp . etc.
In most cases, these pathogens represent the bacteria of the fecal flora, which take the ascending path although in general peristalsis (movements of contractions and distension of the walls of the urinary tract) performs an effective protective action against infections.
Other unusual microorganisms are occasionally reported: mycobacteria, yeasts and fungi, as well as opportunistic pathogens such as Corynebacterium urealyticum .
Risk factors
An anatomical and functional predisposition makes some patients more susceptible to the onset of pyelonephritis. Some of these "critical" factors are: the stagnation of urine, the presence of stones or other renal obstructions (for example: prostatic hypertrophy or tumor), an immunodepression debilitation or peripheral neuropathy (example: spinal cord injury).
Acute and Chronic Pyelonephritis
Pyelonephritis occurs most frequently in acute form, but the recurrence of the infection can lead to chronic pyelonephritis. The two forms of disease are distinguished by the anatomo-pathological aspects and the timing that characterize the infection.
Acute pyelonephritis
Acute pyelonephritis occurs with high fever, back pain in the lumbar region, painful urination, suffering from renal region pressure, nausea and signs of lower urinary tract infection (eg hematuria, dysuria).
The prognosis of the acute form is positive: if adequate therapy is used, the symptoms of pyelonephritis tend to regress approximately in two weeks.
CHRONIC pyelonephritis
Chronic pyelonephritis has less intense symptoms and can be caused by recurrent infections (caused by the same microbial strain) or by reinfections (caused by different microorganisms). The recurrent form of the disease is often responsible for significant inflammatory changes affecting the excretory system. In fact, the evolution of chronic pyelonephritis can induce pionephrosis (severe and extensive kidney disease characterized by the collection of pus, with destruction of the renal parenchyma), urosepsis (systemic inflammatory response propagated from the urinary tract), renal failure and, in the terminal phase, it can even induce the need for an organ transplant .
The diagnostic approach is based on the search for the etiological agent in the urine sample (urine culture + direct microscopic examination ) and on the evidence of an antibody-serum response to the infecting bacteria (common reaction in pyelonephritis).
Treatment
The pathology requires an antibiotic therapy which, if timely, leads to recovery without consequences.
The treatment allows the radical elimination of bacteria that may be present in the urine, by taking specific antibiotic cycles, which also take on a preventive value against the causes and recurrence of the infection. Sometimes, it is necessary to resort to surgery such as urethroscopy (an operative method used, generally, for the treatment of stones, stenoses, small urothelial neoformations) or nephrectomy (partial or total removal of the kidney).
Defense mechanisms of the urinary tract
With the exception of the urethral mucosa, the urinary tract of healthy individuals is resistant to colonization by pathogenic microorganisms, as we have "local" defense mechanisms, in addition to the active participation of the immune system (antibody response, protective role of IgA and IgG ...). Urine is an excellent growth medium for many bacteria, but not for most of the urethral flora (anaerobes, non-hemolytic streptococci, staphylococci) and thanks to its chemical composition, pH and urinary flow it provides effective protection for the excretory apparatus.
It should be noted that the colonization of the urinary tract by pathogenic microorganisms does not always cause infection. In fact, the infectious process depends on:
- charge, virulence and recurrence of microorganisms;
- effectiveness of the host's immune defenses.
In short, the physiological defense of the excretory apparatus is conferred by the following mechanisms:
- Physicists: peristalsis, washing action of urinary flow, cleavage of epithelial cells, stratified epithelium of transition at the level of renal excretory ducts, bladder and initial urethral tract;
- Chemical: acid pH of urine, urea contained in urine (acts as an antagonist with respect to anaerobic bacteria);
- Biological: resident bacterial flora, mucosal resistance to colonization, phagocytosis, mucosal inflammatory response and production of immunoglobulins (IgG, IgA), antibacterial activity of prostatic secretion present in urine, presence in the urine of Tamm-Horsfall protein (secreted by cells tubular, contains mannose and avidly binds Escherichia coli with fimbriae 1, favoring their elimination).