What is the Angina Pectoris
The term Angina Pectoris derives from the Latin terms Angina = pain and Pectoris = chest. It is, in effect, a syndrome characterized by pain in the retrosternal region, sometimes irradiated on the ulnar side of the left arm and at the shoulders.
Causes

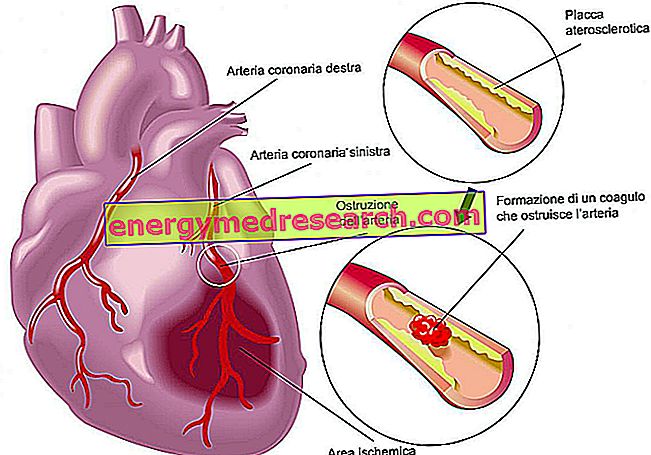
The reversibility of this condition differentiates angina (or angor, which in Latin means suffocation) from the infarct, a much more serious event that is associated with necrosis (death) of a more or less extended part of the heart.
Blood is life, since it carries oxygen and nutrients, giving them to the cells and loading up on waste products. When blood is scarce the tissues suffer and accumulate toxic metabolites. This condition is picked up by the cardiac chemoreceptors and from there sent to the central nervous system which, due to reflex, triggers the pain sensation. The heart is in fact without sensitive nerve endings.
The blood supply to the myocardium can become insufficient compared to the needs of the heart itself already in conditions of rest or during a physical effort (climbing stairs, lifting and carrying an object, heavy etc.). Stress and anger in general can cause the appearance of the disease.
Angina pectoris is a clinical picture characterized by the appearance of chest pain resulting from secondary myocardial ischemia, almost always linked to coronary atherosclerosis.
Classification
Angina can be classified differently depending on whether clinicopro-gnostic, pathophysiological or descriptive criteria are used.
The clinical-prognostic classification of angina is mainly of two types:
- Angina stable (or Angina da Sforzo)
- Unstable angina (or pre-infarct syndrome)
Stable and Unstable Angina
Angina Stabile or Sforzo
CHRONIC syndrome that occurs most frequently as stress, cold or stress angina.
It is the MOST DIFFUSED form of the disease and for this reason it is also called typical angina pectoris. It generally arises during physical efforts and in general in all those situations that require a greater flow of blood to the heart. In these cases the severity of the symptomatology is CONSTANT and does not worsen significantly with the passing of months.
In addition to representing the most widespread form, stable or stress angina is also the least severe, given that acute episodes are predictable in frequency and intensity and for this reason they can be cured with specific medicines that can prevent or stop the attack .
Unstable Angina
It includes different forms of angina pectoris that are linked by the instability of the clinical picture. The two most important characteristics of this form of angina are the recent onset (<1 month) and the ingravescence, or the aggravation in duration and intensity of anginal episodes.
With the passage of time the attacks also manifest themselves for modest physical efforts (reduction of the ischemic threshold), up to appearing already in conditions of absolute rest. In this case the therapeutic control is difficult since the patient himself is unprepared to face the angina attack.
Between the two forms unstable angina is the most dangerous and ranks as gravity between the stable form and myocardial infarction (incidence of AMI in 2% - 15% of cases).
| ANGINA STABILE | UNSTABLE ANGINA |
|
|
Unstable angina in turn is divided into two subspecies:
- silent ischemia
- the variant prinzmetal angina.
ANGINA OR ISCHEMIA SILENTE
It is a transient condition in which a discrepancy occurs between consumption and myocardial oxygen supply. Unlike the other forms of angina, silent ischemia is characterized by the absence of symptoms, and therefore of pain (hence the silent name = silent). This condition, typical of diabetics and those who have already suffered ischemia or myocardial infarction in the past, can therefore only be diagnosed by specific tests.
The real causes of absence of pain have not yet been established with certainty even though they are probably closely related to an increase in the synthesis and secretion of endorphins (endogenous painkillers) by the central nervous system. Even the same heart attack, like silent angina, in about 15% of cases is not painful.
ANGINA PECTORIS VARIANT OR OF PRINZMETAL
This is a rather rare clinical picture, characterized by the appearance of angina at rest and not during demanding physical efforts.
Usually the anginal attack tends to always occur at the same time of day, often at night. The angina pectoris variant is caused by the excessive spasm (contraction shrinkage) of the coronary arteries which in many cases are devoid of arteriosclerotic plaques.
Other forms of Angina
Physiopathological criteria
Based on the pathophysiological mechanisms that determine it, angina pectoris can be distinguished into primary angina and secondary angina.
Primary angina
It is due to a primary reduction in coronary flow. It typically occurs at rest and is due to temporary obstruction of a coronary vessel, caused by coronary spasm, transient coronary thrombosis, or both.
Secondary angina
It arises secondarily to an increase in the demand for oxygen by the myocardium (classically in relation to an effort), which exceeds the possibilities of supply by the coronary flow.
FUNCTIONAL ANGINA
It brings together all those situations in which angina is not caused by a coronary problem but by other diseases that prevent the heart from receiving the right amounts of blood. This group of diseases includes aortic stenosis and insufficiency, mitral stenosis, severe anemia, hyperthyroidism and severe arrhythmias.
Vasospastic angina, favored by cocaine abuse, also falls into this form.
Descriptive criteria
Cold angina
(caused by exposure to low temperatures and due to coronary vasoconstriction and increased blood pressure).
postprandial angina
It usually occurs after modest efforts only when performed after a meal and may suggest the presence of a severe coronary artery disease).
stress angina
Connected mainly to situations of emotional stress.
decubitus angina
Caused by the assumption of the clinostatic position, which increases cardiac work by increasing preload.
SYNDROME X or microvascular angina
It is an anginal syndrome characterized by episodes of myocardial ischemia in the absence of atherosclerotic lesions.
Also in this case there is a dysfunction that causes an excessive spasm (constriction) of the coronary arteries due to alteration of the normal regulation mechanism between vasoconstriction and vasodilation. The small arterial coronary vessels of resistance are affected.
The risk of angina evolving into more serious cardiac events is very low in this case.
Every single anginal attack is generally classified according to its:
- LOCALIZATION: typically referred to the middle-upper retro-sternal region, it can in some cases affect the entire thoracic area and radiate to the neck, mandible, upper left limb, fingers and shoulders.
- QUALITY: oppressive, constrictive, burning or suffocating, ranging from mild to severe, generally not modifiable with respiratory acts and position variation.
- DURATION: from a few seconds to 15 minutes; if the angina-type pains exceed 20-30 minutes it is probably a myocardial infarction.
- FREQUENCY: sporadic, regular, irregular, frequent