What is Celiac Disease?
Celiac disease, also called celiac sprue or gluten enteropathy, is a disease that affects the intestine as the main organ, but which has many important consequences even at a distance, and which depends on an alteration of the immune response by the lymphocytes T of people genetically predisposed against gluten, which is a substance normally ingested in the diet.

According to the annual report of the Ministry of Health to the parliament on celiac disease, related to 2012, the prevalence of this disease in the adult population appears to be around 1% in Europe, with a range of variability ranging from 0.3% in Germany, at 2.4% of Finland. Italy stands at around 0.7%. In 2012, 148, 662 subjects were positive in Italy for the diagnosis of celiac disease, 12, 862 more than the previous year. Within the population the average male to female ratio is 1: 2; this means that for every celiac male there are two females affected by celiac disease.
Causes
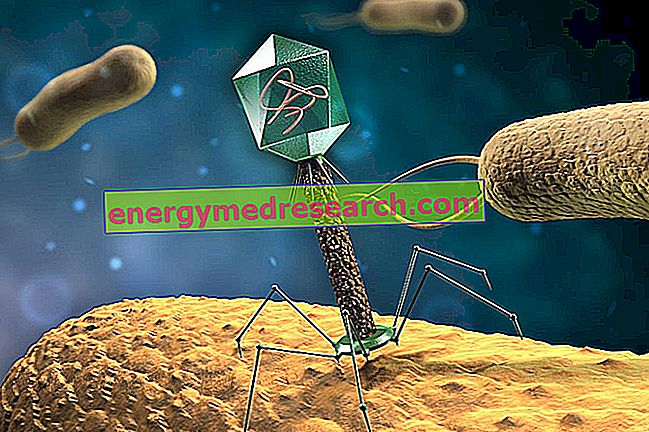
Gluten is a component of wheat, barley and rye (not rice, oats or corn); it contains the protein that is responsible for the inappropriate immune response, which is called gliadin . There are people who, for genetic reasons, are carriers of some variants of what is called Major Histocompatibility Complex Type II (MHC II); these are proteins that cooperate with the immune cells and that would cause the adverse reaction of the immune system itself towards gliadin. Once ingested in the diet, it should be completely degraded by digestive enzymes to obtain individual amino acids. However, it has been discovered that there is a component made of 33 amino acids that resists this degradation and that can pass intact intestinal cells, thus coming into contact with some particular types of cells of the immune system, which present the MHC II molecules on the their surface. These cells internalize within themselves the component of 33 amino acids of gliadin, digest it and dismantle it into smaller particles, which are then returned to their surface and expressed through a bond to class II MHC molecules. The resulting complex has a strong ability to activate T lymphocytes, which thus initiate an immune response that causes local damage, represented by an inflammation that takes place in the intestinal wall, and the activation of B lymphocytes, which produce antibodies against gliadin (anti-gliadin) and other antibodies (called anti-endomysium and anti-transglutaminase), all belonging to the class of immunoglobulins A. Another important consequence that can occur is the induction of a defect in the production of lactase ( an enzyme used to digest lactose), which also involves an intolerance to milk and dairy products, if it was not already present.
Celiac Symptoms
To learn more: Celiac Symptoms
Celiac disease occurs quite often in childhood, but in reality it can occur at any age, so that cases diagnosed after 60 are on the increase. The severity of symptoms depends on the extent of the disease along the intestine, as the less extensive forms, which usually affect only the first portion of the small intestine, can cause nuanced problems that are not immediately attributable to the malabsorption syndrome of celiac disease. For this reason, we recognize a classic form, a subclinical one, and a silent form.
In the classical form there are diarrhea, steatorrhea (feces rich in fat and therefore smelly), weight loss and all those problems that are characteristic of a global malabsorption, especially as regards vitamins, iron and folates. Sometimes, even in the absence of diarrhea, it is quite common to only observe an iron deficiency anemia (more rarely also due to the lack of folic acid and / or vitamin B12) or a aphthous stomatitis (painful ulcers in the oral cavity) that relapse.
The subclinical form of celiac disease is characterized by minor, transient, and apparently extraintestinal symptoms, which only the expert doctor refers to this condition.
The silent form is characterized by the absence of symptoms and signs related to malabsorption.
Both in the established and in the partial forms it is possible that, albeit rarely, phenomena such as increased transaminases, increase in the number of platelets, neurological disorders (alterations of balance, epilepsy), infertility, recurrent abortions, skin alterations such as patches are observed. detected and alopecia. It is therefore appropriate, in the presence of clinical problems of this type that cannot be easily explained, to investigate whether a celiac disease is present.
There is also an association of celiac disease with other pathologies, such as with herpetiform dermatitis, which is a lesion of the skin characterized by very pruritic papules and vesicles located preferentially at the elbows and knees, the trunk and the neck, but also with type I diabetes, autoimmune thyroiditis, Sjögren's syndrome, rheumatoid arthritis, IgA nephropathy, Down syndrome, primary biliary cirrhosis, sclerosing cholangitis, and epilepsy. It is probable that, in these cases, a propensity to autoimmune diseases, in which the subject's immune system rebels against cells of the same subject, determines both the celiac disease and the associated condition.
This pathology can lead to important complications, such as intestinal lymphomas, tumors of the oral cavity, esophagus and small intestine or even significant non-tumor alterations of the small intestine, such as some permanent anatomical alterations of the small intestine structure, making malabsorption not correctable with the elimination from the gluten diet.
Diagnosis
To learn more: Exams for the diagnosis of Celiac disease
The most accurate diagnosis, in a patient with typical symptoms of celiac disease, is performed with an examination called "biopsy of the jejunal mucosa", which reveals the characteristic lesions. It consists in surgically withdrawing a small piece of mucosa from the small intestine (fasting) and observing it under a microscope (histological and cytological examination). The biopsies performed must be two: one preceding the gluten-free diet, showing the typical lesions, and one after a year of gluten-free diet, which must show their significant improvement. The lesions are reversible: in fact, the mucosa returns to have a normal appearance after a few months of gluten-free diet. The biopsy can be performed endoscopically, inserting a thin flexible tube into the patient's mouth and passing it through the esophagus and stomach to the duodenum and fasting; it allows you to perform a targeted extraction at the point where the intestinal wall appears altered. However, there are much simpler methods, using blood samples, which are performed before the biopsy, and which for this reason are much more widely used, even for screening studies. They consist of serum detection of antibodies characteristic of the disease (anti-gliadin, anti-endomysium and anti-transglutaminase). Antibody positivity is not diagnostic, but it is useful to select those patients to undergo intestinal biopsy.
Treatment
To learn more: Celiac Disease Medications
The fundamental therapy is the elimination from the diet of all foods containing derivatives of wheat, barley and rye, replacing them with rice, corn, potatoes, soy or tapioca. At least initially, oats are also best avoided. Also the beer must be eliminated, while it is possible to freely consume wine and liqueurs, including whiskey. Unfortunately, small quantities of gluten can also be found in food additives, emulsifiers or stabilizers, or in drugs (capsules and tablets containing starch), it is therefore advisable to check that any food or medicine does not contain gluten. In the presence of celiac disease, it is appropriate, at least initially, to abstain also from the consumption of milk or dairy products, given that a deficit in intestinal lactase production may also occur.