Generality
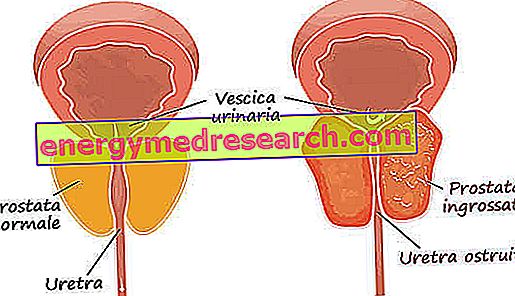
Among the pathologies affecting the prostate, the most common is certainly benign prostatic hypertrophy or adenoma of the prostate. This happens especially after 50-60 years. As the years go by, in fact, the central part of the prostate tends to swell up to even exceed 2-3 times the measures considered normal. The rate of estrogen increases with age and, being the muscular part of the prostate gland with a large number of estrogen receptors, it also increases the risk of hypertrophy. Instead, the absence of correlation with the social and cultural state, blood type, smoking habits, alcohol abuse, cardiovascular diseases, diabetes, liver cirrhosis and hypertension has been scientifically demonstrated. Unlike prostate cancer (which generally originates from the peripheral portion), hypertrophy develops in the central prostate.
Disease development

Symptoms
To learn more: Symptoms prostatic hypertrophy
As already mentioned above, the main symptom of prostatic hypertrophy is the decrease in the size and urinary jet, often associated with difficulty in starting urination. Other symptoms could be: need to urinate more often than normal, nocturia (need to urinate at night), urination urgency (urgent need to urinate, sometimes with involuntary loss of a few drops of pee), "intermittent" urination (more time ), feeling of not having completely emptied the bladder, difficulty starting urination (despite the presence of a strong stimulus), post-urination drip (after urinating, the patient notices the leakage of some drops of urine). In the most serious cases, complete inability to urinate (urinary retention) may also occur, so that the catheter is needed for emptying.
Diagnosis
The first diagnostic test to verify the presence of prostatic hypertrophy is, even today, rectal exploration: a simple, non-invasive and very reliable investigation. The positive outcome of the examination is given by the sight of a hardened, painful prostate and, in case of prolonged obstruction, dilation of the ureters and renal cavities linked to the return of urine from the bladder to the kidney or from the inability to make the urine flows normally towards the bladder. Prostatic hypertrophy must be differentiated from prostate cancer; this makes the role of the doctor of fundamental importance. The urologist, in fact, during the visit must make an accurate differential diagnosis between the two diseases. Other diagnostic tests are: PSA (prostate specific antigen), a blood test that is used to assess the concentrations of the prostate antigen; urinalysis (to ascertain the presence of leukocytes: white blood cells that indicate the presence of an infection); ultrasound urology (study of the state of the kidneys, bladder and prostate by means of a probe connected to an apparatus, called an ultrasound system), to be performed with a full bladder.
Therapy
drugs
To learn more: Drugs to treat Benign Prostatic Hypertrophy
In the case of mild (or first-degree) hypertrophy, the urologist generally prefers only medical intervention, which uses the following drugs: the 5 alpha reductase inhibitors and the alpha-lithics.
The first group of drugs (in particular finasteride and dutasteride ) acts by stopping the transformation of testosterone into its active form dihydrotestosterone, which stimulates prostate growth.
The alpha-lithicians, on the other hand, belong to the class of drugs able to relax the muscles of the bladder neck, the prostatic urethra and the prostate itself, thus facilitating the passage of urine into the urethra.
However, both groups of drugs may have side effects . In particular, 5 alpha reductase inhibitors can reduce the erectivity of the penis, while alpha-lithics can reduce arterial pressure and, only rarely, generate retrograde ejaculation (sperm emission "in reverse", towards the bladder instead of on the outside). All these effects, however, disappear when treatment is stopped.
Phytotherapy
To learn more: Treating prostatic hypertrophy with herbs
In addition to the aforementioned drugs, there are also some plant substances and extracts (Nettle, African pygmy, pumpkin seeds, serenoa repens) that appear to have an anti-inflammatory and decongestant effect on the prostate.
Surgical intervention
To learn more: TURP - Transurethral resection of the Prostate
If the hypertrophy is moderate or severe, the urologist almost always prefers surgical treatment, which can make use of two methods: the endoscopic and the classical surgical procedure (reserved, now, only for patients with very voluminous prostate or with particular characteristics). The operation in endoscopy today represents the most widespread intervention for this type of pathology. In general, over 90% of patients may undergo endoscopic prostate resection or TURP (Trans Urethral Resection of Prostate). The advantage is better acceptance by the patient, as no incision is required. An instrument called a resector is used, which is introduced into the urethral canal. Thanks to a lens on the device, the doctor is able to observe the inside of the urethra and to identify the two prostatic lobes that occlude the canal, which will be cut into small pieces and finally extracted. In this way the urethral canal is widened and cleared. The internal wound usually heals after 2-3 days of catheter, used to drain urine. Other endoscopy interventions are TUIP and TULIP. The first is the incision of the prostate, through deep cuts that allow to enlarge the central and obstructive part of the prostate; the second is, instead, the transurethral incision by means of laser and photocoagulation. This last technique is particularly indicated for those patients who present a high risk of bleeding
BPH
X Problems with video playback? Reload from YouTube Go to Video Page Go to Wellness Destination Watch the video on youtube