Paclitaxel (or taxol) is an anticancer drug belonging to the class of antimitotic agents. It is a natural taxane and was first isolated from a North American conifer, Taxus brevifolia .

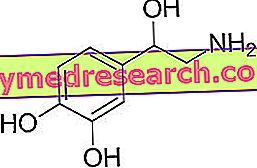
Paclitaxel - Chemical Structure
Indications
For what it uses
The use of paclitaxel is indicated for the treatment of the following diseases:
- Metastatic breast cancer;
- Ovarian cancer;
- Non-small cell lung cancer;
- Pancreatic cancer;
- Kaposi's sarcoma related to AIDS.
Warnings
Paclitaxel should only be administered by specialized personnel under the strict supervision of a doctor experienced in administering anticancer agents.
Since paclitaxel causes myelosuppression (bone marrow suppression), the hematological parameters must be frequently monitored.
Care should be taken when administering paclitaxel in patients with heart disease; therefore, frequent checks of vital signs are recommended.
Patients with hepatic impairment are more exposed to the risk of paclitaxel-induced toxicity, especially there is an increased risk of developing myelosuppression.
Great caution should be used when administering paclitaxel in patients with the following conditions:
- Uncontrolled ongoing infections;
- Reduced kidney function;
- Pre-existing peripheral neuropathy;
- Modifications of the CBC test;
- Severe inflammation of the mucous membranes.
Interactions
In combination therapy with cisplatin (an anticancer medicine), paclitaxel should be administered before the latter.
Paclitaxel should be administered 24 hours after the use of doxorubicin (an antitumor antibiotic), so as to avoid an increase in the plasma concentration of the same.
In the case of concomitant administration of drugs used to treat HIV (such as - for example - efavirenz, nevirapine, ritonavir and nelfinavir ), a dose adjustment of paclitaxel may be necessary.
A dose reduction of paclitaxel may be required if erythromycin (an antibiotic), fluoxetine (an antidepressant) or gemfibrozil (a drug used to lower cholesterol levels) is administered simultaneously.
In the case of concomitant administration of paclitaxel and rifampicin (an antibiotic used to treat tuberculosis) an increase in the dose of paclitaxel administered may be necessary.
Caution should be used in concomitant administration of paclitaxel and drugs used to treat epilepsy - such as, for example, carbamazepine, phenytoin or phenobarbital - as these drugs affect the elimination of paclitaxel.
Side effects
Paclitaxel can induce many side effects, although not all patients experience them. The type of adverse effects and the intensity with which they appear varies from individual to individual, depending on the different sensitivity that each person has towards the drug.
The following are the main side effects that may occur following treatment with paclitaxel.
Myelosuppression
Treatment with paclitaxel may induce myelosuppression. This suppression causes a decrease in blood cell production which can lead to:
- Anemia (decrease in hemoglobin blood levels), the main symptom of the onset of anemia is the feeling of physical exhaustion;
- Leukopenia (decreased white blood cell levels), with increased susceptibility to contraction of infections;
- Plateletopenia (decrease in the number of platelets), this leads to the appearance of bruising and abnormal bleeding with an increased risk of bleeding.
Gastrointestinal disorders
Paclitaxel therapy can cause nausea, vomiting and diarrhea.
Vomiting can occur from a few hours to a few days after taking the drug and can be controlled by using anti-emetic drugs.
Diarrhea, on the other hand, can be treated with anti-diarrheal drugs. In some cases, however, diarrhea can occur in severe form accompanied by fever and stomach pain.
In any case, it is good to drink a lot to replenish lost fluids.
In addition, the drug can cause intestinal obstruction or perforation, inflammation of the colon, pancreatitis, esophagitis and constipation.
Oral cavity disorders
Treatment with paclitaxel may promote the development of oral ulcers, dry mouth and pain. To prevent these symptoms, take plenty of fluids and clean your teeth regularly with a soft toothbrush.
A temporary loss of the sense of taste that is usually regained at the end of therapy may also arise.
Lung and respiratory tract disorders
Paclitaxel can cause tightness in the chest, lack or difficulty in breathing, upper respiratory tract infections, pulmonary embolism, pulmonary fibrosis, interstitial pneumonia, dyspnea, cough and pleural effusion.
Alopecia
Treatment with paclitaxel can cause hair and hair loss in general. This side effect usually disappears shortly after the end of treatment.
Cardiac disorders
Paclitaxel therapy may induce palpitations, atrial fibrillation, supraventricular tachycardia, heart attack, atrioventricular block and heart failure.
Vascular pathologies
Paclitaxel can cause high blood pressure and encourage thrombus formation. However, the drug could also cause hypotension.
Skin and subcutaneous tissue disorders
Treatment with paclitaxel may trigger skin reactions, pruritus, erythema, urticaria and exfoliative dermatitis. More severe reactions may also occur, such as Stevens-Johnson syndrome (a more severe variant of polymorphic erythema) and toxic epidermal necrolysis.
In addition, paclitaxel can cause nail changes that can also come off.
Hepatobiliary disorders
Paclitaxel therapy may promote jaundice and impair liver function. Hepatic necrosis and hepatic encephalopathy may also occur, both of which can be fatal.
Ear disorders
Paclitaxel can cause reduction or loss of hearing and tinnitus (ie the perception of buzzing, whistling, hissing, tinkling, etc.).
Eye disorders
Treatment with paclitaxel may cause disorders of the optic nerve, inflammation of the eyes and visual disturbances.
Other side effects
Other side effects that may occur following the use of paclitaxel are:
- Allergic reactions in sensitive subjects, sometimes even very serious and accompanied by anaphylactic shock;
- Hot flashes;
- Edema;
- Dizziness;
- Muscle pains;
- Joint pains;
- Temperature;
- Chills;
- Headache;
- dizziness;
- Confusional state;
- Fatigue;
- Peripheral neuropathy (a disease affecting the peripheral nervous system);
- Phlebitis;
- Increased sweating;
- Syncope;
- Backache;
- Chest pain;
- Anorexia;
- Tumor lysis syndrome (syndrome caused by the release into the bloodstream of substances contained in tumor cells, following their lysis);
- Macular edema;
- Scleroderma;
- Systemic lupus erythematosus.
Overdose
There is no specific antidote in case of overdosage with paclitaxel, therefore the treatment is symptomatic. However, since the drug is administered only by specialized personnel, it is very unlikely that overdose will occur.
Action mechanism
Paclitaxel is a taxane with antimitotic action. More precisely, it is a promoter of tubulin polymerization.
Antimitotic agents exert their action during cell division ( mitosis ), in particular, during the phase in which the newly synthesized DNA must divide between the two daughter cells.
The breakdown of the genetic material takes place thanks to the mitotic spindle, a complex structure consisting of microtubules. Microtubules are structures that are formed following the polymerization of a particular protein, tubulin.
Paclitaxel establishes links with the tubulin that constitutes the microtubules, stabilizing them and preventing their disassembly. In this way, a morphological alteration is created which leads the cancer cell to undergo apoptosis (a mechanism of programmed cell death).
Mode of Use - Posology
Paclitaxel is available for intravenous administration. It appears as a viscous, colorless or yellow liquid.
It can be administered through three different routes:
- Through a cannula (a thin tube) that is inserted into a vein of an arm or hand;
- Through a central venous catheter that is inserted subcutaneously into a vein near the clavicle;
- Through the PICC line (Peripherally Inserted Central Catheter), in this case, the catheter is inserted into a peripheral vein, usually of an arm. This technique is used for the administration of anticancer drugs for a prolonged time.
The dosage of paclitaxel must be established by the doctor depending on the type and severity of the tumor and depending on the body surface and the patient's condition. Furthermore, the dose of paclitaxel can be changed depending on whether the drug is given as monotherapy or in combination therapy with other chemotherapy drugs.
Pregnancy and breastfeeding
Due to the serious congenital anomalies that paclitaxel can cause in the newborn, pregnant women should not take the drug.
Furthermore, adequate precautions must be taken by patients and their partners to avoid the onset of pregnancy. The precautions must be taken both during the treatment and for a period of at least six months from the end of the same.
Breast-feeding mothers should not take paclitaxel. If paclitaxel therapy is needed, breastfeeding should be stopped. Breastfeeding cannot be resumed until the doctor has given his consent.
Contraindications
The use of paclitaxel is contraindicated in the following cases:
- Known hypersensitivity to paclitaxel;
- Excessively low white blood count;
- In the presence of a serious and uncontrolled infection when the drug is to be used for the treatment of AIDS-related Kaposi sarcoma;
- Pregnant;
- During breastfeeding.