Generality
Tenosynovitis is an inflammation that affects the synovial sheath, that anatomical structure that lines the tendon to reduce friction from rubbing along its course.
Typically, a tendon affected by tenosynovitis is affected simultaneously by tendonitis : the site of maximum inflammation is the synovial lining, but the inflammatory response can also involve the included tendon.
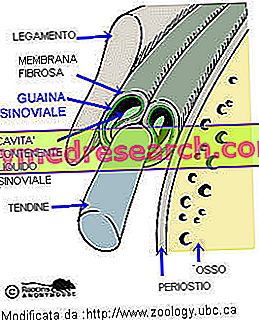
The inflammatory process of the synovial sheath causes an increase in the volume and viscosity of the synovial fluid, which generates friction, therefore pain and limitation of movements
The inflammatory process that affects the tendon sheath manifests itself with pain, difficulty in movement and production of fluid that can generate swellings (swellings) appreciable from the outside.
The main causes that determine the onset of tenosynovitis are prolonged traumas or functional stresses, rheumatic diseases or infections. The most affected sites are the hands, the wrist, the forearm, the instep and the Achilles tendon. The inflammation makes the sheath wrinkled and irregular (example: crackling tenosynovitis, associated with a crackling that accompanies the movement of the affected joint) or harsh, often with the consequent formation of a nodule (snap tenosynovitis).
Among the most common tendon synovitis we mention the chronic stenosing thumb tenosynovitis (also called De Quervain syndrome), the tenosynovitis of the anterior tibial and stenosing tenosynovitis of the finger flexors (commonly called "snap finger").
Note . In the terminology there is often confusion between tendinitis and tenosynovitis . The term tendinitis indicates an inflammation of the tendon, but this, being very little vascularized, compact and poor in cells, cannot develop a classic inflammatory picture.
The damage to the fibers leads only to edema and to regressive alterations; the most explicitly phlogistic phenomena remain localized to the relative synovial sheath that covers the tendon (tenosynovitis).
Causes
The exact etiology of tenosynovitis is unknown, but can be traced to mechanical causes, such as excessive physiological use of tendons or abnormal stresses (excessive strain).
Slight trauma repeated over a long period of time may increase the damage to the synovial sheath. Some competitive sports (tennis, walking, skating etc.) and the repeated use of hand tools in some professions can promote the onset of tendon synovitis.
Tenosynovitis is also linked to systemic diseases such as rheumatic diseases and infections mediated by pathogenic microorganisms, which penetrate due to wounds or the spread of infectious processes (for example: osteomyelitis, paterecules ...). In these infectious forms of tendon synovitis, the inflammatory process can assume suppurative characters (with formation of pus within the inflamed tissue).
Infectious tenosynovitis in brief
Infectious tenosynovitis is caused mainly by streptococci: bacteria reach the tendon due to a deep wound or diffusion of infectious processes in adjacent anatomical areas. The symptoms are intense pain (often pulsating), swelling and redness. The therapy is based on taking antibiotics and possibly on the surgery of the tendon sheath to eliminate the collection of pus.
Symptoms
To learn more: Symptoms Tenosynovitis
The disease is characterized by pain, reduced movement in the affected region and, in case of snap tenosynovitis, by sudden blockage of the tendon during movement.
The sheaths can accumulate synovial fluid and cause swelling, or they can generate friction, felt with a stethoscope (during the medical examination, when the tendon moves inside its sheath).
Localized pain may be present along the course of the tendon.
The sites most frequently affected by tenosynovitis are:
- the capsule of the shoulder joint and the tendons associated with it (rotator cuff);
- the radial and ulnar flexor of the carpus;
- the flexors of the fingers;
- the capsule of the hip joint and the tendons associated with it;
- the Achilles tendon;
- the long adductor and the short extender of the thumb, which divide a common fibrous sheath (De Quervain syndrome).
Diagnosis
The physical examination is divided into the following phases: inspection, movement, palpation and specific tests. The medical examination allows to detect the swelling near the involved joint and to evaluate the pain and the manifestation of the symptomatology correlated to the functional stress. The tendon affected by synovitis appears to be oedematous on palpation (in the inflamed point, the slight compression on the tendon causes pain). If it is possible, the doctor can give passive movements to the joints with his fingers, to feel any painful lumps.
The ultrasound allows to detect the edema, a diffuse tendon alteration and sometimes a effusion that wraps the tendon itself. Moreover, the ultrasound examination allows to distinguish the different forms of tenosynovitis (for example: the increase of exudative fluid inside the synovial sheath in De Quervain syndrome or the presence of synovial tissue hypertrophy in proliferative tendon synovitis). A complementary support, to make the diagnosis, can also be provided by magnetic resonance imaging and an X-ray examination. These diagnostic investigations allow to highlight alterations due to traumas and to identify possible calcium deposits in the tendon and its sheath.
Treatment
Treatments aimed at tendon synovitis depend on the severity of the inflammation and the location in which it is located, but in most cases allow complete recovery.
The goals of the therapy are:
- relieve pain;
- reduce inflammation;
- restore joint function.
Therapeutic management includes:
Medical treatment
The main cure is based on physiotherapy and rest, which is essential for recovery. In cases of acute inflammation, the patient can apply cold packs to the area affected by tenosynovitis. Mild forms of the disease can be treated with non-steroidal anti-inflammatory drugs (NSAIDs) and local analgesic drugs for about 7-10 days. The most serious cases are treated with cortisone infiltrations and, subsequently, with paracetamol and ibuprofen. For the complete resolution of the inflammatory process related to tendon synovitis symptomatic therapies and infiltrations may be necessary every 2-3 weeks for one or two months.
Infiltrative therapy in tenosynovitis
In relation to the severity and location of the pathological process it may be useful to perform infiltrations with a corticosteroid (example: dexamethasone acetate, methylprednisolone acetate or hydrocortisone acetate) near the site where there is greater pain.
Administration by injection must be performed very carefully, to prevent the liquid from coming into contact with the tendon, since it can cause weakening or breakage of the tendon.
Rehabilitative therapy
Physical therapy can be useful to reduce the symptoms and special exercises can be indicated, in relation to the patient's tolerability, which make the joint affected by tendon synovitis progressively more active (physical exercise is particularly useful to prevent the so-called frozen shoulder, following the resolution of the inflammation).
Surgical approach
If tenosynovitis is persistent and resistant to therapy, surgical arthroscopy and the removal of calcium deposits may be considered, followed by gradual physiotherapy. The surgical approach is rarely necessary and usually involves the surgical release or removal of the altered synovial sheaths (sineviectomy).



