Generality
Myoclonus are involuntary muscle contractions, similar to shocks, which appear in a brusque and lightning manner. This movement disorder depends on an over-stimulation generated by the nervous system.

The myoclonus can be found both in physiological situations, and in the context of many pathological pictures of varying extent and nature.
Distinctive elements of myoclonus are the sudden presentation (shock-like) and the relatively short duration . This sort of muscle shake with an irregular or rhythmic pattern can occur singularly or repetitively, with an average frequency of 10-50 contractions per minute. Myoclonus simultaneously affect one or more muscles in a single body region, in contiguous or distant districts.
Myoclonic episodes can be triggered by an external event, such as a specific movement or a sensory stimulus. In fact, however, myoclonus remains spontaneous and uncontrollable (involuntary) reactions.
Massive (or generalized) myoclonias involve the whole body and are more frequently observed in diseases of the central nervous system of degenerative origin and in some forms of epilepsy . Myoclonic shocks can also be found in cases of traumatic brain damage, ischemic stroke, viral infection of the brain, tumors, Alzheimer's, toxic-metabolic disorders and unwanted reactions to drugs .
Examples of physiological myoclonus are, instead, the hiccups, the flickering of the eyelids and the jerks of the legs that can appear before falling asleep .
Regarding treatment, medical intervention is not always necessary. If the diagnostic procedure ascertains the presence of a basic pathology, the therapeutic management of the latter can be useful to keep symptoms under control, including myoclonus. When the cause is unknown or the disorder cannot benefit from a specific cure, the treatment is symptomatic and aims exclusively to alleviate the consequences on the patient's quality of life.
What are
Definition of Mioclonus
Myoclonus is defined as a movement disorder characterized by a rapid, sudden and involuntary series of muscular contractions . Their manifestation involves one or more muscles at the same time.
Myoclonus can occur singly (i.e. in isolation) or in sequence, rarely or repeatedly repeated per minute. In most cases, the muscles of the extremities or the trunk are involved .
Myoclonus can manifest itself in both positive and negative form:
- POSITIVE MYCHLONIES : in most cases, myoclonus occurs in a positive form, ie as active muscle contractions;
- NEGATIVE MIOCLONIA : less often, myoclonus is manifested as an interruption or inhibition of muscular activity in progress, perceived as a sudden relaxation or a fall in postural tone.
Myoclonus: characteristics
By definition, myoclonus is a short-term, abrupt and sudden (shock-like) movement disorder. These involuntary and lightning-fast muscle contractions are generated by the nervous system. Myoclonus have modalities of variable presentation and heterogeneous etiologies.
From the clinical point of view, myoclonus can be classified according to:
- Appearance method :
- Spontaneous myoclonus : they occur in the absence of triggering factors;
- Myoclonus induced by a stimulus :
- Action myoclonus : they are triggered by a specific movement that requires muscle coordination. In extreme cases, the sole intention of performing the movement may be sufficient for the appearance of myoclonus. The causes of myoclonus action are, in general, brain damage caused by hypoxia, ie lack of oxygen during breathing or temporary lack of blood flow to the brain due to cardiac compromise;
- Reflex myoclonias : they are induced by emotional, mental and / or sensory stimuli (tactile, visual or auditory);
- Spatial distribution :
- Focal myoclonias : affect the musculature of a single region of the body, usually distal in distribution;
- Segmental myoclonias : they occur at the level of two or more contiguous regions;
- Multifocal myoclonus : they involve, asynchronously, different body areas;
- Generalized myoclonus: also called massive myoclonus, involving, in an apparently synchronous way, many areas or the whole body. Generalized myoclonias are found mainly in epilepsy, in virus encephalitis and in brain anoxia following cardiac arrest (in the latter case, myoclonic shocks are continuous);
- Frequency :
- Irregular : myoclonus can occur singularly or in a non-repetitive manner;
- Periodic : myoclonus recur with a certain frequency, on average with 10-50 contractions per minute.
Furthermore, based on temporal distribution, myoclonus can be classified as synchronous or asynchronous .
Terminology and synonyms
When we talk about myoclonus, we refer to a clinical sign and not to a disease; specifically, it is a series of muscular contractions, perceived by the patient as rapid, sudden and involuntary shocks. Myoclonus belong to the broader category of movement disorders, that is, the set of conditions characterized by a dysfunction of voluntary musculature.
Myoclonus are also called myoclonic or myochemical spasms .
In addition to myoclonias, tremor, bradykinesia, choreoathetosis, tics, synkinesis and dystonia are also part of the movement disorders category.
Causes
Physiological mechanisms of myoclonus
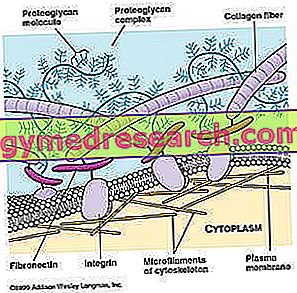
Myoclonus is generated by the nervous system and depends on a state of neuronal hyper- excitation .
From the neurophysiological point of view, it is possible to distinguish:
- Cortical myoclonus;
- Cortico-subcortical myoclonus;
- Subcortical-supraspinal myoclonus;
- Spinal myoclonus;
- Peripheral myoclonus.
Cortical myoclonias are characterized by very brief tremors, while the subcortical ones are relatively long.
The mechanisms underlying some forms of myoclonus are not yet fully known. At present, it has been hypothesized that some types of stimulus-sensitive myoclonus may be related to an over-excitability of parts of the brain and spinal cord that are responsible for controlling the movement of voluntary muscles.
In determining this state of over-stimulation, some neurotransmitters are likely to play a role, making some cells more sensitive. Serotonin and gamma-aminobutyric acid (GABA) seem to be implicated in the phenomenon of myoclonus, which help the brain to control muscles.
Mioclonus: types
Considering the numerous pathologies that can represent a clinical manifestation, myoclonus have conventionally been divided into four categories:
- Physiological myoclonus : these are involuntary contractions related to particular events, such as hiccups, states of anxiety, prolonged exertion, sleep, excessive consumption of caffeine and fatigue. In most cases, physiological myoclonias are transient and have no pathological or worrying significance;
- Essential myoclonias: they occur as an isolated manifestation, in the absence of a degeneration of the central nervous system (note: essential myoclonias are not usually associated with epileptic seizures and neurological deficits);
- Epileptic myoclonias : they occur in extremely heterogeneous clinical pictures, in which the predominant element is a specific form of epilepsy;
- Symptomatic myoclonias : they are manifested in diseases of the central nervous system (CNS) of degenerative, toxic-metabolic origin, from hypoxic or traumatic damage. Symptomatic myoclonias are also those that appear in the course of systemic metabolic or toxic diseases, such as hypoglycemia, liver decompensation, renal failure, electrolyte imbalance or drug intoxication.

Myoclonus: main pathological causes
In pathological conditions, myoclonus occurs within:
- Diseases of the central nervous system (CNS) of degenerative origin:
- Parkinson's disease;
- Huntington's Korea;
- Some forms of dementia:
- Alzheimer's;
- Creutzfeldt-Jakob disease;
- Brain damage from:
- Ischemia (eg stroke, tumors, etc.);
- Hypoxia (prolonged reduction of oxygen supply to the brain);
- Traumas with cerebral or spinal cord injuries (in particular, areas in charge of controlling the musculature affected by the disorder);
- Multiple sclerosis;
- Epilepsy (some forms, in particular: idiopathic generalized epilepsy with myoclonus, continuous partial e., Infantile myoclonic, progressive or benign myoclonic, etc.);
- Viral encephalopathies:
- Herpes simplex encephalitis;
- Toxic encephalopathies:
- Exposure to DDT and heavy metals;
- Metabolic disorders or systemic toxicosis, such as:
- Hypercapnia (increase in the blood concentration of carbon dioxide);
- Hypoglycemia (low blood sugar concentration);
- Hepatic decompensation;
- Kidney failure;
- Uremia;
- Side effect or drug intoxication.
Examples of physiological myoclonus
One of the best known examples of myoclonus are the trembling eyelids : the flickering of the palpebral lines is induced by the involuntary contraction of one of the eye muscles for reasons such as excessive fatigue, stress and lack of sleep.
In physiological conditions, myoclonus can occur during the initial phase of sleep, before falling asleep ( hypnic myoclonus ).
Myoclonus induced by drugs or other substances
Myoclonus can be iatrogenic, that is caused by side effects of some substances and drugs in high doses, such as:
- Antihistamines;
- Some antidepressants (eg amitriptyline);
- Bismuth;
- Levodopa;
- Opiates.
Symptoms and Complications
Myoclonus is felt as a rapid, sudden and uncontrolled shock. These movements can affect a muscle or a group of muscles regardless of their functional association (ie not necessarily involved in the same movement). Massive myoclonias can involve the entire body.
In their simplest form, these spasms alternate phases of contraction (positive myoclonus) with relaxation phases (negative myoclonus). In most cases, myoclonus involves the muscles of the extremities or trunk.

Most common presentation method
- The typical presentation of myoclonus is in the form of paroxysms at irregular intervals, during functional rest or not. The typical muscular movement is a sudden contraction (positive myoclonus) or a weakening of the muscle tone (negative myoclonus), but can also occur asterissi or "flapping tremors", that is short inhibitions of contraction.
- Myoclonus occur in a single episode or, more often, repeating in series even 10-50 contractions in a minute;
- Myoclonus is reduced during voluntary movement and increases during muscle relaxation. The extent of this activity is generally sufficient to produce a net movement of the joints with spasms at the ends.
- Normally, myoclonus disappear during sleep, but a series of such contractions can also appear at the beginning of sleep ( hypnic myoclonus ).
Symptoms associated with myoclonus
Physiological myoclonias usually appear as an isolated and short-lived phenomenon (from a few seconds to a few hours). Occasionally, episodes may occur for a few days, resulting in quite annoying.
Generalized or massive myoclonias involve all or most of the body, mostly spontaneously and intermittently or continuously; clearly, these shocks can interfere with everyday life, hindering activities such as eating, sleeping, talking and walking.
The symptoms associated with myoclonus vary depending on the cause and the district involved.
In general, these episodes may be related to:
- Muscle weakness;
- Tachycardia;
- Sweating;
- Insomnia;
- Muscle cramps;
- Hyporeflexia (diminished reflexes).
Myoclonus can be a harmless and transient phenomenon, due to an easily solved condition. However, the problem is worrying when it is presented consistently in frequency and duration.
Diagnosis
Myoclonus is an objective finding, the recognition of which can be carried out by the doctor during the patient's physical examination. The identification of the exact cause that triggers myoclonic episodes, however, is not always so immediate; the diagnostic procedure involves several diagnostic investigations to exclude or confirm the clinical suspicion.
Myoclonus: what tests are needed for diagnosis?
The evaluation of myoclonus involves a careful anamnesis (information relating to the illnesses of which one is suffering, modalities of onset of the symptom etc.) and a physical (neurological) examination, to determine the causes and / or establish the presence of underlying pathologies.

Based on the outcome of these initial investigations, the doctor may prescribe further investigations, such as:
- Blood tests : measure blood levels of sugar, calcium, magnesium or sodium. Abnormal levels of these substances may indicate that the cause of myoclonus is a metabolic disorder. In the context of blood chemistry tests, liver and renal function tests can also be performed, as well as toxicological investigations to rule out any organ insufficiency or substance abuse;
- Magnetic resonance imaging (MRI) : diagnostic imaging examination that allows the central nervous system (encephalon and spinal cord) to be viewed and the presence of any lesions, tumors and compromises of areas that can induce myoclonus to be assessed;
- Electromyography (EMG) : it allows to verify muscle contraction under electrical stimulation by means of electrodes and provides details on the correct functionality of both skeletal muscles and peripheral nerves (ie outside the brain and spinal cord). Electromyography is useful for identifying the nerve endings involved in myoclonus, which the patient suffers from;
- Electroencephalogram (EEG) : can be indicated to check for the presence of myoclonus in those suffering from seizure disorders.
Treatment
To intervene in the most correct way, it is important to identify the exact cause that triggers myoclonus. In any case, it is always advisable to contact your doctor for the most suitable indications for the specific situation.
- Physiological myoclonias must be considered above all as a passing and non-pathological phenomenon; rarely, these spasms are so severe as to require emergency treatment.
- When myoclonus is the expression of a specific and reversible condition - usually with an external origin in the nervous system, as in the case of metabolic disorders - the treatment is aimed at the underlying disease.
- The myoclonus that occurs in specific pathological conditions can be alleviated with conservative therapies or targeted surgical procedures. For example, in the presence of a brain tumor or spinal cord injury, it may be necessary to undergo surgical treatment.
Pharmacological therapy of myoclonus
At present, some causes of myoclonus cannot be definitively resolved: in these cases, a symptomatic type of therapy is important, that is that it tends to decrease and keep the problem under control.
The doctor may prescribe some medicines, chosen on the basis of criteria linked to the type of myoclonus or underlying disease. In most cases, to control myoclonic episodes, anti-convulsants, muscle relaxants or anti- epileptics are indicated.