Epidemiology
The duodenal ulcer is 4-10 times more frequent than the gastric ulcer. It can appear at any age, but the peak of maximum incidence is found between 30 and 40 years. It is more common in males, with a male / female ratio of 3: 1. According to some statistics it is thought that around 10% of the population develops a duodenal ulcer in the course of life. Unlike the gastric one, the duodenal ulcer has no differences in incidence linked to the socio-economic condition.
Causes
Also for duodenal ulcer, no specific causes of onset are known. The factors assumed as responsible are instead multiple. It is believed that the main one is represented by acid hypersecretion . This seems to depend substantially on the numerical increase in acid-secreting cells of the gastric mucosa, from the increase in gastric response to secretory stimuli and from the altered ability to inhibit gastrin release. Furthermore, patients with duodenal ulcer have a more marked response than healthy subjects and gastric ulcer carriers to stimulation by gastrin; this may be indicative of an increased response capacity of the parietal cells to it. Even a particularly intense vagus nerve stimulation could play a significant role in inducing acid hypersecretion.
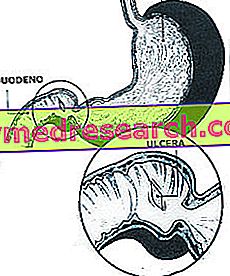
Form and location of the ulcerative lesion
95% of duodenal ulcers are located in the duodenal bulb, within 3 cm of the pylorus. The front wall of the bulb is the most frequently affected site; they follow in order of frequency the posterior wall and the superior and inferior margins of the bulb. The average diameter of duodenal ulcers is about 1 cm. The morphology is similar to that of gastric ulcer. Complications are bleeding, perforation and stenosis (occlusion); the possibility of evolution in a malignant tumor would seem to be excluded.
Due to the thinness of the duodenal wall, ulcers of the anterior wall of the bulb can undergo perforation with a certain ease.
The ulcers of the posterior wall of the bulb tend instead to penetrate into the head of the pancreas, due to the close proximity of the two organs and can lead to the development of inflammatory reactions of the pancreas itself (acute pancreatitis). The hemorrhagic complications of the duodenal ulcer can be fatal, because the deepening of the ulcer can lead to the erosion of important arterial branches
Symptoms and diagnosis
To learn more: Duodenal Ulcer Symptoms
Although some patients with active duodenal ulcers are free of symptoms, usually the presence of the ulcer is characterized by epigastric pain, sometimes referred to as a sense of annoyance or hunger, but more often defined as deaf and constricting. In some cases the pain is located to the right of the median abdominal line, and may radiate to the right shoulder or to the dorsal and lumbar region.
This latter irradiation is often a sign of the deepening of the duodenal ulcer in the head of the pancreas. The pain typically appears from 1 hour and a half to 3 hours after the meal ( late postprandial ), and in more than half of the cases it causes the patient to wake up at night. The intake of food and antacid drugs, involves the resolution of the pain in a short time. There may be episodes of nausea and vomiting. The symptomatology tends to be episodic and recurrent.
Typical is its seasonal exacerbation in spring and autumn. Symptomatic periods lasting a few days or weeks alternate with remissions that can last several months or years.
Patients who are at the same time suffering from gastric ulcer and duodenal ulcer, usually have symptoms mainly referable to that of the duodenal ulcer.
Diagnosis
The differential diagnosis must be placed with gastritis, duodenitis, chronic inflammation of the gallbladder due to stones, biliary colic, pancreatic diseases and, rarely, with hepatitis.
Confirmation of the presence of duodenal ulcer is provided by endoscopic examination (gastroduodenoscopy) or by radiological examination with baritized meal.



