Generality
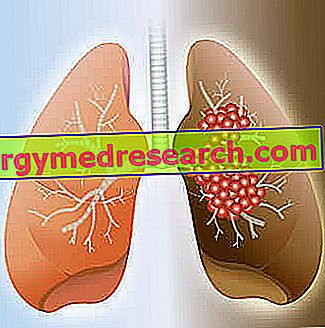
Small cell lung cancer (SCLC) is a tumor process characterized by high malignancy.
Initial symptoms of small cell lung cancer include persistent cough, difficulty breathing and chest pain. The diffusion by contiguity to neighboring structures can cause, instead, hoarseness, dysphagia and superior vena cava syndrome, due to the compressive effect on the part of the neoplastic mass.
The onset of small cell lung cancer is closely related to cigarette smoking and is rarely found in a person who has never smoked.
Small cell lung cancer is often characterized by very rapid growth, so it can spread outside the chest quickly, causing widespread metastases. For these reasons, it is not generally susceptible to surgical therapy.
Causes
Small cell lung cancer is characterized by the uncontrolled growth of bronchial lining epithelial cells .
Also called oat grain tumor or microcytoma, this carcinoma owes its name to the small size of the tumor cells observable under a microscope.
In fact, small cell lung cancer is made up of tumor clones with poor cytoplasm and well-defined margins, rounded or oval, sometimes lymphocyte-like. Furthermore, some types of SCLC can have spindle or polygonal elements.
Cancer cells organize themselves into groups or masses that do not show glandular or scaly architecture. Furthermore, some of these neoplastic clones have neurosecretory granules ( cells of the APUD system ).
The pathogenic event triggering the onset of small cell lung cancer is to be found in the mutation of genes that stimulate cell growth (cMyc, MYCN and MYCL) and the inhibition of apoptosis (BCL-2). Further involved elements are the onco-suppressors (p53), whose inactivation justifies the peculiar neoplastic progression of this type of tumor.
In any case, before becoming neoplastic, respiratory epithelial cells need prolonged exposure to carcinogens and accumulate multiple genetic aberrations.
Epidemiology
About 15-20% of lung cancer cases are of the small cell type; all other cancers are "non-small cells".
SCLC occurs almost always in smokers and occurs, above all, in middle-aged people (27-66 years).
Risk factors
- Tobacco smoke. Cigarette smoking is undoubtedly the main risk factor for the development of small cell lung cancer; only in a minority of cases, the neoplasm arises in non-smokers. The risk varies according to the intensity and duration of this habit and can decrease after the cessation of the habit, but it can never be comparable to that of those who have never smoked. The onset of the tumor can also be favored by passive smoking .
- Professional risks. In smokers, the risk of small cell lung cancer is higher in the case of combined exposure to ionizing radiation or to certain substances (for example: asbestos, bis-chloromethyl ether, coal fumes, silica, cadmium, chromium and nickel) at work.
- Air contamination. Other risk factors involved in the development of small cell lung cancer include exposure to radon gas, a product of the decay of natural radioactive elements present in soil and rocks, such as radium and uranium, which can accumulate in enclosed areas. Even air pollution can increase the risk of developing this type of cancer.
- Familial and previous pulmonary diseases. Some respiratory tree diseases (such as tuberculosis, COPD and pulmonary fibrosis) may increase lung cancer susceptibility, as well as a positive family history for this form of cancer (especially in parents or siblings) and previous treatments of radiotherapy (used, for example, for a lymphoma).
Signs and symptoms
Compared to other lung cancers, small cell cancer is highly malignant, therefore it is extremely aggressive and spreads very quickly.
The symptomatology is caused by local invasion of the tumor, the involvement of adjacent organs and metastases .
Cancer cells can migrate through the lymph nodes to the lymph nodes or through the bloodstream.
In several cases, small cell lung cancer is asymptomatic in its early stages or causes non-specific manifestations; sometimes, the disease is accidentally detected during diagnostic examinations for chest images performed for other reasons.
Local tumor
The most common symptoms associated with local cancer are:
- Cough that does not tend to resolve after two or three weeks;
- Breathing difficulty (dyspnea);
- Sputum, with or without traces of blood (hemoftoe);
- Vague or localized chest pain;
- Shoulder pain.
Paraneoplastic syndromes and systemic symptoms can occur at any stage of disease and may include:
- Recurrent or persistent fever, usually, not very high;
- Unexplained fatigue;
- Weight loss and / or loss of appetite.
Paraneoplastic syndromes are characterized by symptoms that occur in areas distant from a tumor or its metastases.
In patients with small cell lung cancer, it is mainly possible to find:
- Syndrome of inappropriate antidiuretic hormone secretion (SIADH);
- Lambert-Eaton syndrome (LEMS);
- Cushing syndrome.
Regional dissemination
Small cell lung cancer can spread contiguously to neighboring structures (such as pleura lining the lungs, pericardium or chest wall).
The regional spread of cancer can cause:
- Chest pain due to pleural irritation;
- Dyspnea due to the development of a pleural effusion;
- Difficulty or pain when swallowing (dysphagia);
- Hoarseness;
- Hypoxia for diaphragmatic paralysis due to phrenic nerve involvement.
Pericardial tumor spread may be asymptomatic or cause constrictive pericarditis or cardiac tamponade.
Hemoptysis is a less frequent manifestation and blood loss is minimal, except in the rare case where the tumor infiltrates a main artery, causing massive bleeding and death due to asphyxia.
Upper vena cava syndrome
The appearance of the superior vena cava syndrome occurs due to compression or invasion of the superior vena cava by the tumor. This condition can lead to headaches, facial and upper extremity edema, dilatation of the veins in the neck, dyspnoea in the supine position and flushing of the face and trunk.
metastasis
The disease easily causes metastases outside the chest, so other symptoms may be present, secondary to the spread of the tumor at a distance. These manifestations vary according to their location and may include:
- Liver metastases : pain, jaundice, gastrointestinal disorders and organ failure.
- Brain metastases: behavioral changes, paresis, nausea and vomiting, convulsions, confusional state, aphasia, up to coma and death.
- Bone metastases : severe bone pain and pathological fractures.
Almost all organs can be affected by metastasization of small-cell lung cancer (including liver, brain, adrenal glands, bones, kidneys, pancreas, spleen and skin).
Possible complications
Small cell lung cancer is the most aggressive form of lung cancer ever. About 60% of patients have metastatic disease at the time of diagnosis.
Diagnosis
The diagnostic path must begin with an accurate medical history and a complete physical examination, to identify symptoms and typical signs of the disease.
The limited sensitivity of chest radiographs does not allow early identification of small cell lung cancer. Therefore, the alterations found on the radiographic examination (such as a solitary pulmonary mass or nodule, a hilar enlargement or a tracheobronchial narrowing) require further evaluation, usually with computerized tomography (CT) or PET-CT (an investigation that combines anatomical study of CT with functional imaging of positron emission tomography). PET images can help differentiate inflammatory processes and malignant lesions, as well as highlighting thoracic diffusion and the presence of distant metastases.
The diagnosis requires a cytopathological confirmation by percutaneous biopsy, bronchoscopy or thoracoscopic surgery and subsequent histological examination, ie the microscopic study of the sample taken. The cytological examination of the fragments of suspect tissue thus collected allows to search for cellular lesions typical of small-cell lung cancer.
Staging
Based on metastasis, small cell lung cancer can be distinguished in 2 stages of staging: locally delimited and advanced.
- By locally delimited disease we mean a tumor confined to one of the hemithoraxes (including the ipsilateral lymph nodes), which can be included in a tolerable radiotherapeutic field, in the absence of pleural or pericardial effusion.
- On the other hand, the advanced disease is a cancer that extends beyond a hemithorax; furthermore, malignant cells can be found in pleural or pericardial effusion.
Less than a third of patients with small cell carcinoma present with limited stage of disease; the remaining patients often have extra-thoracic tumor foci.
Treatment
At any stage, small cell lung cancer is initially sensitive to treatment, but the responses are often short-lived.
The most effective approach in prolonging survival and improving patients' quality of life involves the use of radiotherapy and / or chemotherapy .
Generally, surgery is only indicated in selected cases and is performed very rarely. Given the characteristics of small cell lung cancer, in fact, this approach has no role in treatment, although resection of the involved lung area may be decisive in cases where the patient presents a small focal tumor without diffusion (like, for example, a solitary pulmonary nodule).
Regarding the treatment of this type of lung cancer, biological therapies based on drugs that have a precise molecular target are still under study.
Chemotherapy and radiotherapy
The chemotherapy strategy usually used for small cell lung cancer involves a combination of etoposide and a platinum compound (cisplatin or carboplatin). Therapeutic protocols with topoisomerase inhibitors (irinotecan or topotecan), vinca alkaloids (vinblastine, vincristine and vinorelbine), alkylating drugs (cyclophosphamide and ifosfamide), doxorubicin, taxanes (docetaxel and paclitaxel) and gemcitabine may also be used.
In limited-stage disease, radiation therapy combined with chemotherapy further improves the response. In some cases, cranial irradiation should be considered to prevent brain metastases . The risk of micrometastasis to the central nervous system within 2-3 years from the start of treatment is in fact high and, unfortunately, chemotherapy is not able to cross the blood-brain barrier.
In more advanced cases, the treatment is based on chemotherapy, rather than on radiotherapy, although the latter is often used for palliative purposes (ie to reduce symptoms), in the presence of bone or brain metastases.
It is not yet clear whether replacing etoposide with topoisomerase inhibitors (irinotecan or topotecan) can improve survival. These drugs alone or in combination with others are normally used in refractory disease and recurrent cancer at each stage.
Prognosis
The prognosis for small cell lung cancer is unfortunately unfavorable. The median survival time for limited small cell tumor disease is 20 months, with a 5-year survival rate of 20%. Patients with small cell tumors with diffuse disease, on the other hand, have a particularly poor prognosis, with a 5-year survival rate of less than 1%.
Prevention
With the exception of smoking cessation, no active intervention has proven efficacy on the prevention of small cell lung cancer.
In summary: characteristics of small cell lung cancer
- Synonyms: small cell lung cancer (SCLC), microcytoma or oat grain tumor .
- % of lung carcinomas : 15-20% of cases.
- Location : airway submucosa; mass in hilar or central lung region.
- Risk factors : smoking (essentially all patients); possible environmental and professional exposure (asbestos, radiation, radon and passive smoking).
- Complications : common cause of superior vena cava syndrome; paraneoplastic syndromes and diffuse metastases.
- Treatment : chemotherapy (pharmacological combinations using etoposside, irinotecan or topotecan plus carboplatin or cisplatin); radiotherapy; no major role for surgery.
- 5-year survival after treatment : limited tumor: 20%; widespread: <1%.