Generality
Prostatitis is the inflammation of the prostate gland, that is the purely male organ, shaped like a chestnut, located just below the bladder and having a decisive role in the formation of the sperm.
There are 4 types of prostatitis:
- acute prostatitis of bacterial origin (or type I prostatitis),
- chronic prostatitis of bacterial origin (or type II prostatitis),
- chronic non-bacterial prostatitis (or type III prostatitis)
- asymptomatic prostatitis (or type IV prostatitis).
To identify the precise type of prostatitis, an accurate diagnosis is required, which includes tests on blood, urine and sperm samples and prostatic fluid.
The treatment of prostatitis varies according to the causes and characteristics of the inflammation of the prostate gland; for example, the presence of a prostatitis of bacterial origin requires the planning of a suitable antibiotic therapy.
Prostate: outline of anatomy and functions
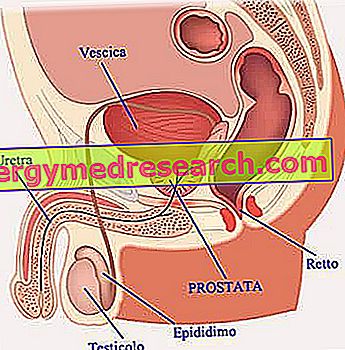
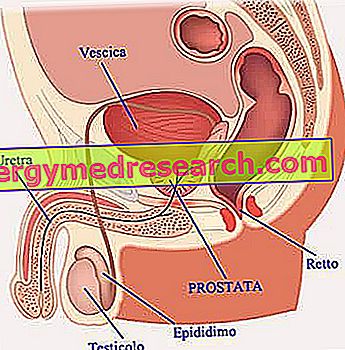
The prostate (or prostate gland ) is a purely male gland, located just below the bladder, in front of the large intestine portion called the rectum . In shape and size, it looks a lot like a chestnut.
Part of the urethra runs through the prostate, ie the duct that carries urine outside and - at the moment of orgasm - the seminal fluid (NB: see the following part dedicated to the functions).
Around the prostate, muscles called sphincters take place, the contraction of which makes urine output momentarily impossible, while allowing the release of sperm ( ejaculation ).
FUNCTIONS
The prostate secretes a particular liquid, called prostatic fluid, which - when mixed with other secretions (for example the liquid produced by the seminal vesicles ) and with the spermatozoa - constitutes the aforementioned seminal fluid (or sperm).
Prostatic fluid is vitally important for spermatozoa originating in the testicles, as it guarantees their nourishment, protection (when and if they are inside the uterus) and increased motility.
What is prostatitis?
Prostatitis is inflammation of the prostate or prostate gland.
It is not a neoplasm - so it should not be confused with prostate cancer - and it is not even an abnormal enlargement of the prostate (a condition which in medicine is called benign prostatic hypertrophy or enlarged prostate ).
Types of prostatitis
In 1999, the so-called National Institute of Diabetes and Digestive and Renal Diseases (based in the United States) defined 4 types of prostatitis:
- Acute prostatitis of bacterial origin or type I prostatitis ;
- Chronic prostatitis of bacterial origin or type II prostatitis ;
- Chronic prostatitis of non-bacterial origin or type III prostatitis or chronic pelvic pain syndrome .
- Asymptomatic prostatitis or type IV prostatitis .
Once known as prostatodynia, this type of prostatitis can be distinguished by a marked or small inflammatory nature. In the first case (marked inflammatory nature), it is also called chronic inflammatory pelvic pain syndrome or type IIIA prostatitis ; in the second case (irrelevant inflammatory nature), however, it is better known as chronic non-inflammatory pelvic pain syndrome or type IIIB prostatitis .
Epidemiology
Prostatitis can affect any male individual; however, statistical data in hand, is more frequent in the male population aged between 30 and 50 years (the peak is around 40 years).
Acute bacterial prostatitis
Acute prostatitis of bacterial origin - also known as type I prostatitis or acute bacterial prostatitis - is inflammation of the prostate, rapid and sudden appearance, caused by bacteria .
Causes
The bacteria that cause acute prostatitis of bacterial origin can be:
- The same bacteria that cause urinary infections, in other words the bacteria that cause cystitis (bladder infection), urethritis (urethra infection), etc.
In such situations, the development of acute prostatitis may depend on a phenomenon of the spread of bacterial pathogens by blood (through the blood) or direct (from contiguous regions).
- The same bacteria that induce sexually transmitted infections, or bacteria that give rise to chlamydia, gonorrhea, etc.
Normally, in these circumstances, the triggering event is an anal intercourse or a series of anal intercourse with an infected person: bacterial pathogens come from the large intestine of the subject carrying the infection, and colonize the prostate of the healthy individual, going up through the urethra (upward contamination).
- The bacteria that generally inhabit the rectum (eg, Escherichia coli ).
Given the proximity between rectum and prostate, these bacteria can, following particular conditions (eg, an intestinal lesion), escape from their typical site and colonize the adjacent prostate gland.
Other causes
Acute prostatitis of bacterial origin can also be the consequence of: an epididymitis (inflammation of the epididymis ), phimosis (abnormal shrinkage of the foreskin), an obstruction of the bladder neck, an injurious trauma at the level of the perineum (area between scrotum and anus) or a prostate biopsy (in these situations the inflammation is a complication of the procedure in question).
What is a prostate biopsy?
Prostate biopsy is the diagnostic test that involves the collection of a sample of prostate cells and the subsequent analysis, in the laboratory, of the aforementioned sample, in order to confirm or exclude the presence of a prostate carcinoma (a malignant tumor).
Risk factors
They are risk factors for acute bacterial prostatitis:
- The presence of a bacterial infection in the urinary tract (cystitis, urethritis, etc.);
- Drink a little water. It is a risk factor for bacterial infections in the urinary tract; therefore, in male individuals, it is also a risk factor for acute prostatitis of bacterial origin;
- Unprotected sexual relations with people suffering from a sexually transmitted infection;
- Having multiple sexual partners;
- Bladder catheterization;
- A previous prostate biopsy intervention;
- The presence of lesions at the level of the rectum;
- The immunosuppression. People in a state of immunodepression (the so-called "immunosuppressed") are subjects with reduced immune defenses or totally lacking in immune defenses, which makes them susceptible to the repeated development of bacterial, viral and / or fungal infections.
Two major causes of immunodepression are AIDS and diabetes;
- The presence of an orchite, or an inflammation of one or both testicles;
- The stress.
Symptoms and complications
To learn more: Symptoms Prostatitis
As a rule, acute prostatitis of bacterial origin begins in an abrupt and sudden way, typically manifesting itself with:
- High fever with chills;
- Flu-like symptoms;
- Feeling very sick;
- Localized pain in the pelvic area, the lumbar area of the back, around the anus, groin and / or scrotum;
- Urinary problems such as
- Sensation of urgent need to urinate,
- Nocturia (need to urinate at night),
- Dysuria (difficult urination, not necessarily accompanied by pain),
- Hematuria (blood emission with urine),
- Stranguria (intermittent or slow, and painful urination),
- Smelly urine emission,
- Reduced urinary flow
- Difficulty in completely emptying the bladder.
- Pain during sex intercourse;
- Painful ejaculation;
- Pain during defecation and feeling sick during bowel movements;
- Hemospermia (blood in sperm)
Less common symptoms of acute bacterial prostatitis
Sometimes, acute bacterial prostatitis is responsible for widespread muscle pain and widespread joint pain.
Complications
Acute prostatitis of bacterial origin represents an emergency condition, from which various complications can arise.
Among the complications of an untreated, or late treatment, acute bacterial prostatitis include:
- The chronic nature of inflammation at the prostate level;
- The transmission of bacterial infection to nearby anatomical structures, such as the testicles, and the development of conditions, such as epididymitis, orchitis, etc .;
- The passage of bacterial infection to the blood, with consequent development of bacteremia or, in the most unfortunate cases, sepsis ;
- The formation of a prostatic abscess (an abscess is a circumscribed collection of pus);
- The inability to urinate.
There is no scientific evidence to support the thesis that acute prostatitis of bacterial origin would favor the development of some neoplasia of the prostate.
When should I go to the doctor?
A man should contact his treating physician immediately and request a check-up if he is a victim of:
- High fever with chills, associated with an unusual pain in the pelvic area, groin and / or scrotum;
- Episodes of painful ejaculation;
- Urinary problems (only one or more than those mentioned above).
Diagnosis
In general, the diagnostic procedure for the detection of acute bacterial prostatitis, and its precise causes (the triggering bacterium) of origin, begins with an accurate physical examination and a careful medical history; therefore, it continues with the so-called digital rectal exploration ( ERD ) and palpation of the inguinal lymph nodes; finally, it ends with: blood tests, urine tests, laboratory tests on a sample of prostatic fluid obtained after prostate massage, spermioculture, urethral swab, urodynamic examination, cystoscopy and ultrasound of the urinary tract.
The use of such a complex series of diagnostic investigations also serves to exclude conditions from symptoms similar to acute bacterial prostatitis (differential diagnosis).
Blood and urine tests
Blood and urine tests are used to detect the presence of pathogens in them.
These tests are easy to perform, completely painless and inexpensive.
Semen
Spermioculture is the laboratory diagnostic test that allows to detect the presence and type of any pathogenic microorganisms, inside a sperm sample.
Spermioculture is a useful investigation to identify infections affecting the organs in which sperm and seminal fluid flow, namely: the prostate, the seminal vesicles, the epididymis and the urethra .
It is an easy test (it requires some preparatory rules, but they are all very simple) and painless.
Urethral swab
The urethral swab is the diagnostic test of choice for the detection of infectious agents in the lower urinary tract, particularly in the urethra.
It is particularly indicated in the detection of Neisseria gonorrhoeae (the causative agent of gonorrhea ) and Chlamydia trachomatis (the causative agent of chlamydia ).
The urethral swab requires simple preparation and tends to be bothersome.
Urodynamic examination
The urodynamic examination is a diagnostic test that studies and evaluates the functionality of the bladder and urethra, during the respective tasks of storage (bladder) and release (urethra) of urine.
As a rule, doctors use one or more urodynamic tests in the presence of urinary problems (pain during urination, urgent urination to urinate, etc.) and urinary tract infections.
Bacteria that most commonly cause acute bacterial prostatitis:
- Bacteria belonging to the genus Proteus
- Bacteria belonging to the genus Klebsiella
- Escherichia coli
Therapy
The treatment of acute prostatitis of bacterial origin consists of an antibiotic therapy .
Since the prostate is not very sensitive to the action of antibiotics, this therapy must last for several weeks, so that it has the desired effects (that is, it determines the elimination, from the organism, of the causative infective agent).
What is the precise duration of antibiotic therapy?
To learn more: Drugs for the treatment of prostatitis
Generally, antibiotic therapy for acute bacterial prostatitis lasts 4 to 6 weeks ; it is not excluded, however, that the treating doctor decides to prolong it a few more days, if he has legitimate doubts about the resolution of the infection.
Regarding the duration of antibiotic therapy, for an acute bacterial prostatitis the doctors are quite clear and state that the treatment should be continued until the disease has completely disappeared; very importantly, treatment should never be interrupted by simple regression of symptoms (a phenomenon that can occur even after a few days of therapy).
The regression of symptoms, in fact, does not mean having eliminated the infective agent from the body .
Early discontinuation of antibiotic therapy for acute bacterial prostatitis exposes to relapses .
A very common mistake
Stopping antibiotic therapy in the face of a regression, sometimes even a striking one, of symptoms is a very common mistake committed by people with acute bacterial prostatitis.
Treatment of complications
The formation of a prostatic abscess requires the use of surgery, to drain the pus.
Bacteremia and sepsis require further antibiotic treatment, to be added to that against pathogens responsible for acute prostatitis, and to be performed in a hospital setting under the strict supervision of a doctor. In fact, bacteremia and sepsis represent two health emergencies that require the immediate intervention of specific personnel who are experts in the field.
Finally, the inability to urinate forces patients to use the bladder catheter to empty the bladder.
How to behave during the treatment phase
During the treatment phase of acute bacterial prostatitis, doctors recommend patients to drink plenty of water (to avoid dehydration due to fever) and to abstain from sexual activity (NB: the partner must also undergo antibiotic therapy). In addition, they advise (or deem useful to speed up healing):
- Masturbation, because ejaculation favors the emptying of the prostate and the removal of the bacteria that have infected it;
- Abstention from cycling at any intensity (therefore even the simple bike ride to the city center), because sitting on the bike's saddle involves pressure on the prostate;
- The use of a cushion to sit on (the ideal would be a donut pillow);
- Hot baths;
- A diet that excludes the consumption of substances such as coffee, alcohol and spices, as they are considered "irritants".
See the deepening: Diet and Prostatitis
Other possible drugs
In some circumstances, in addition to antibiotic therapy, doctors could prescribe other pharmacological treatments, including:
- A treatment based on alpha-blocker drugs. Alpha blockers have the effect of releasing the smooth muscles of the bladder and prostate; this, in people with benign acute prostatitis, should lead to a reduction in urinary problems.
Among the alpha-blockers most used in the presence of acute bacterial prostatitis are: doxazosine, terazosin and tamsulosin.
- A treatment based on pain-relieving drugs, ie pain medications. The classic painkillers prescribed for acute prostatitis of bacterial origin are paracetamol and ibuprofen (an NSAID).
Prognosis
The prognosis for acute bacterial prostatitis depends on the timeliness of diagnosis and treatment, which must be adequate.
The timely identification of the condition and its immediate and adequate treatment almost always involve the positive resolution of the inflammatory state; on the contrary, late detection of the disease and / or neglect of treatment tend to have, due to consequences, the chronic nature of inflammation, bacteremia, increased risk of relapse and other complications discussed.
Prevention
To prevent acute bacterial prostatitis, we recommend
- practice a healthy and safe sexual activity,
- take liquids (water) in quantities appropriate to the body's needs,
- take care of intimate hygiene,
- avoid activities that can cause perineal trauma
- to treat urinary tract infections promptly.