Generality
Bone marrow transplantation, also called hematopoietic stem cell transplantation, is the therapeutic treatment with which a sick bone marrow is replaced with another healthy one, in order to restore normal blood cell production.
The procedure is very complex and, in order for it to be carried out, it requires different conditions: among all of them, a good patient's state of health (in spite of the illness that afflicts him) and the impracticability of any other alternative intervention.

Figure: hematopoiesis starting from totipotent stem cells. From these derive different types of stem cells, including hematopoietic ones. Hematopoietic stem cells have the gift of continually replicating and of choosing whether to become red blood cells, white blood cells or platelets. From the site: www.liceotorricelli.it
The risks associated with the procedure are numerous and by no means negligible. Therefore, before proceeding with a bone marrow transplant, it is good to make sure that there are all the ideal conditions for its implementation.
Brief reminder of what bone marrow is and how it works
Bone marrow is a soft tissue, present in the internal cavity of some bones (femur, humerus, vertebrae, etc.)
Its job is to produce blood cells, namely red blood cells (erythrocytes), white blood cells (leukocytes) and platelets (thrombocytes). This maturation process is called hematopoiesis (or hematopoiesis ) and starts from particular cells, called hematopoietic stem cells . The latter are real progenitor cells, able to replicate continuously and to meet different destinies.
- Red blood cells : they carry oxygen to the tissues and organs of the body.
- White blood cells : they are part of the immune system and defend the body from pathogens and from what can harm you.
- Platelets : they are among the main actors of coagulation.
What is bone marrow transplantation
Bone marrow transplantation, also known as hematopoietic stem cell transplantation, is the medical procedure by which a damaged bone marrow is replaced by another healthy bone marrow from a healthy donor.

Why do we practice?
Bone marrow transplantation is used to treat all those pathological conditions or diseases that damage the bone marrow, to the point of making it unable to produce functioning blood cells.
The classic situations, which may require the execution of a bone marrow transplant, are:
- Aplastic anemia
- Leukemia
- Non-Hodgkin's lymphoma
- Genetic diseases of the blood or immune system
With the insertion of a healthy bone marrow, it is intended to restore normal hematopoiesis and recover the function of blood cells.
What happens if:
- The red blood cells are missing, the circulating blood is poor in oxygen, therefore the individual feels tired and his organs are destined to a slow deterioration.
- White blood cells are missing, the risk of infections increases dramatically.
- Platelets are missing, it increases the ease with which one goes towards bleeding and hematoma.
APLASTIC ANEMIA
The continuous exchange of erythrocytes, leukocytes and platelets, performed by the bone marrow, allows an individual to lead a healthy life. Conversely, a bone marrow unable to perform this function causes a pathological condition, called aplastic anemia .

LEUKEMIA
Leukemia is a tumor of white blood cells, which reproduce uncontrollably and no longer fulfill their protective function. Furthermore, their number, inside the blood vessels, becomes so high that it prevents erythrocytes and platelets from remaining at normal quantitative levels (anemia and thrombocytopenia).
There are different types of leukemia:
- Acute lymphoblastic leukemia
- Acute myeloid leukemia
- Chronic lymphocytic leukemia
- Chronic myeloid leukemia
LYMPHOMA NON-HODGKIN
Non-Hodgkin's lymphoma is also a white cell tumor, but unlike leukemias (which spread in the bloodstream), it affects the lymphatic system .
The lymphatic system is a collection of vessels and organs ( lymph nodes ), disseminated throughout the body, which protect the body from infections and foreign agents.
GENETIC DISEASES OF BLOOD AND IMMUNE SYSTEM
Some blood diseases, such as sickle cell disease or thalassemia, and the immune system, such as primitive immunodeficiencies, can be caused by a genetic DNA mutation, present since birth.
Transplant candidates
What is the best patient to receive a transplant?
The aforementioned pathological conditions are not always resolved with a bone marrow transplant. In fact, since the latter is a treatment not free from risks and complications, certain conditions must be present, in order to put it into practice.
- The patient, who needs a transplant, must be fine, in spite of the illness that afflicts him (for example, those who, suffering from cancer, find themselves in the remission phase).
- The patient has a brother or sister who can act as a bone marrow donor. As will be seen later, members of the same family (or blood relatives) possess a very similar medullary tissue, therefore the risk of rejection is less.
- The disease, which afflicts the patient, has not responded positively to any alternative and less dangerous treatment than bone marrow transplantation.
- The risk / benefit ratio favors the latter.
HLA TYPES
What makes it clear if the tissues and organs of two different people are similar? How do you identify an ideal bone marrow donor?
In the tissues and organs of each of us, there is a genetic mark, equivalent to a badge, called HLA (from the English Human Leukocyte Antigen ). This HLA is usually extremely different from individual to individual, but in some cases it can be very similar. When there is similarity between HLA, we talk about compatibility . The compatibility of HLA is one of the conditions necessary for an organ transplant to be successful.
Ideal bone marrow donors, therefore, must have, in the cells of their organs and tissues, an HLA implant compatible with that of the recipients.
In which people is it easier to find HLA compatibility?
The blood relatives, especially the siblings, probably have similar HLA, if not equal.
To be sure, it is sufficient to perform specific tests on the two brothers (the healthy and the sick) and compare the resulting HLA.
BONE MARROW REQUEST
Who is an only child or has no siblings with a compatible HLA can only apply for bone marrow, by joining a waiting list . In this case, the bone marrow can come from any person with a similar HLA and regularly registered with the donor registry .
The wait, unfortunately, can last even years, with more than dramatic consequences on the requesting patient.
CAN ALL MAKE BONE MARROW DONORS?
To register in the donor register you must:
- Be at least 18 years old, for legal reasons, and no more than 40 years, for medical reasons. A donor can be called until they reach the age of 55.
- Weigh more than 50 kg
- Enjoy good health and do not suffer from any infectious disease
Preparation and procedure
Bone marrow transplantation is a very long procedure that can be divided into 5 phases (or stages). In chronological order:
- Physical examination of the patient
- Harvesting (or taking) of the bone marrow to be transplanted
- Conditioning
- Hematopoietic stem cell transplantation
- Period of restoration (or healing)
PHYSICAL EXAMINATION
For bone marrow transplant to be successful, it is essential that the patient is well, despite the illness that afflicts him.
Therefore, with a careful physical examination, the most important internal organs are analyzed, such as the heart, liver and lungs: their state of health provides the doctor with all the useful information, to know how the entire organism will respond to drugs for the conditioning phase.
Two special cases where physical examination is very important:
In the case of infections . After the transplant, the patient is exposed to infections, as he must take immunosuppressants to reduce the response of the immune system and, with it, the possibility of a rejection. For this reason, knowing if the patient suffers from an infectious disease before transplantation has an essential value.
In the case of tumoral pathologies . In this case, a biopsy is performed, ie the collection and analysis of a sample of tumor cells. If the examination shows that the neoplasm is in remission, then it is possible to proceed with the transplant and hope for a success of the latter; vice versa, if the neoplasm is still in the acute phase, transplantation is not recommended, because it may not have any valid result.
BONE MARROW COLLECTION
If the physical examination has given a positive response, proceed with the collection of the bone marrow to be transplanted.
It can occur in two ways: by a classic method or by a recently introduced method.
- Classic method (or donation of traditional bone marrow) . It consists of the direct collection, through a syringe, of the bone marrow present at the level of the iliac crests. The donor is subjected to general anesthesia and the intervention lasts about 45 minutes. The content of removed bone marrow varies according to age; however, in general, it is around one liter. After the collection, the donor is kept under observation for at least 24 hours and he is advised to rest for the next 4-5 days. The only hazards and undesirable effects of the procedure are related to general anesthesia and the painful sensation that is created at the level of the sampling area. It is a widely applied method among young donors.
- Non-traditional method (or donation of hematopoietic stem cells from peripheral blood) . In the 5 days prior to bone marrow donation, the donor is subjected to a pharmacological treatment that favors the production of hematopoietic stem cells and their passage into the circulating blood. Once the necessary time has elapsed, this blood is taken from an arm, passed through a special machine, which separates the stem cells from the rest of the blood and collects them separately, and re-infused immediately into the donor, through the other arm. It is a procedure that lasts about 4 hours (it is performed in a day-hospital) and with minimal side effects (headache, bone pain, etc.), which is put into practice especially among adult donors. If the doses of hematopoietic stem cells taken are insufficient for a transplant, a second sample should be taken after at least 6 days.
Due to the extreme difficulty in finding a bone marrow suitable for each patient, an alternative transplantation strategy has been developed to the so-called allogeneic one, in which the bone marrow comes from another person. This is an autologous transplant, whose execution requires that the bone marrow be taken directly from the patient to be treated.
NB: for a complete description of what allogeneic transplantation and autologous transplantation are, see the subchapter dedicated to the actual transplant procedure.
CONDITIONING
The conditioning phase is, in fact, a preparatory phase for the actual transplant.
It consists of a pharmacological treatment, chemotherapeutic and / or radiotherapeutic, aimed at three different objectives:
- Destroy the patient's bone marrow, to leave space for the new one to be inserted
- Destroy all the neoplastic cells, present in the bone marrow, which could influence the good execution of the transplant (NB: this objective is valid if at the origin of the bone marrow disorders there is a neoplasm)
- Limit the response of the immune system so as to reduce the chances of rejection.
Conditioning usually lasts 4 to 7 days and requires the patient to stay in the hospital.
Some side effects of conditioning chemotherapy:- Nausea
- He retched
- Diarrhea
- Loss of appetite
- Buccal ulcers
- Fatigue
- Skin rash
- Hair loss
- Lung disorders
- Hepatic disorders
TRANSPLANTATION OF HEMATOPOIETIC STEM CELLS
The transplant operation must be performed one or two days after the conditioning phase.
Hematopoietic stem cells, however they are taken, are infused into the patient, through a large vein that flows towards the heart (for example, the subclavian vein ). This is chosen as an injection point, as a matter of practicality.
The entire process can last from a minimum of an hour and a half to several hours, depending on the condition of the patient and the bone marrow.
Transplantation, in itself, is not painful.
The autologous and allogeneic transplants are described below; what distinguishes these two methods, as anticipated, is solely the origin of hematopoietic stem cells.
- Autologous transplantation . The bone marrow comes directly from the patient to be transplanted. This procedure allows to avoid the long waiting times and all the risks related to compatibility, as it infuses a substance that already belongs to the patient.
In order to carry out this procedure, it is necessary that the bone marrow is still functioning or can be made so. For example, in cases of leukemia, once taken, it is subjected to cycles of radiotherapy and chemotherapy, to clean it from the cancer cells present.
Benefits: reduces waiting time for bone marrow; absolute compatibility; risk of minimal rejection.
Disadvantages: in cancer, it is necessary that the tumor is in remission, otherwise chemotherapy and / or radiotherapy have a limited effect.
Age limit: 60-70 years.
- Allogeneic transplantation . We proceed with allogeneic transplantation, or with the removal of bone marrow from another person, when the patient's is not suitable for autologous transplantation. According to Anglo-Saxon statistics, in only 30% of the cases, the sick have a compatible sister or brother, while in the remaining 70% they have to register on a waiting list. The withdrawal procedure can be either the classic one or the non-traditional one.
Advantages: the bone marrow comes from a healthy person.
Disadvantages: long waiting times (if there are no compatible brothers) and risk of rejection.
Age limit: 55 years.
RESTORATION PERIOD (OR HEALING)
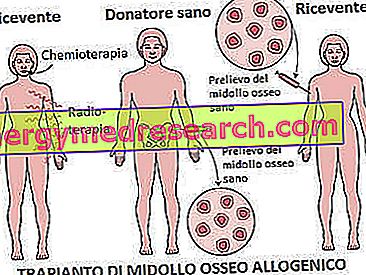
Figure: example of allogeneic bone marrow transplantation. In this case, the removal of healthy bone marrow is performed at the level of the iliac crests, using the traditional method. From the drugs.com website
During the recovery period, a hospitalization of several months is foreseen (even more than three, in exceptional cases).
In the first 15-30 days, the transplant takes place, or the first production, by the new bone marrow, of effective blood cells.
During this time, the patient regularly receives blood transfusions; it must be kept isolated from any possible source of infectious agents and, finally, subjected to a treatment based on antibiotics, as it has a very low number of leukocytes (these are the effects of chemotherapy).
Once taking root, a treatment based on immunosuppressants (and, sometimes, corticosteroids ) must be started, which continue to keep the immune defenses low (leukocytes, etc.), to prevent the possibility of bone marrow rejection.
Frequently asked questions about the hospitalization period:
How long is the patient at risk of infection?
For one or two years, depending on how the patient reacts to the transplant.
Does the patient need nutrition aids immediately after surgery?
Yes, it may need to be nourished by a nasogastric tube, in order to guarantee it all the fundamental nutrients it needs in this delicate phase of treatment.
Can the patient receive visits when he is in the hospital?
Yes, family visits are granted, provided they take all the necessary precautions: the risk, in fact, that the visitor inadvertently brings with him pathogens is high.
risks
Bone marrow transplantation is a risky and uncomplicated therapeutic treatment. This is why, before proceeding with its execution, it is good to inform the patient of all the possible consequences that it may have.
The main dangers consist of:
- Rejection of transplanted bone marrow, also called transplant disease against the host
- Recurrent infections
TRANSPLANT DISEASE AGAINST GUEST OR REJECTION
The rejection, or the aggression by the immune system against the new transplanted bone marrow, is, by far, the most serious complication of the entire treatment.
It can be of two types:
- Transplant disease against the acute type of host . It usually develops in the first three months after surgery and causes high fever (38 ° C), diarrhea, stomach cramps, jaundice and red spots on the hands, feet and face (skin rash).
- Transplant disease against the chronic type of host . It is thus defined when its ailments last for years and appear, generally, several months later (at least three) the intervention. The most frequent complaints are itching, hardening of the skin, xerostomia, dry eyes and hair loss.
When the transplant disease against the host becomes very serious, it can alter the liver functions (ie the liver) and the lungs, with dramatic consequences for the transplanted patient.
The only remedy, put into practice to avoid rejection, is represented, as has already been said several times, by a pharmacological treatment based on immunosuppressants and corticosteroids.
INFECTIONS
The high risk of contracting infections is linked to treatments to prevent rejection.
The most feared infections are lung infections ( pneumonia ).
WHEN ARE THE DANGERS MINOR?
The dangers are reduced, if:
- The patient is young. Studies have shown that bone marrow transplants performed on young people are more successful than those on older people.
- The donor is a brother or sister.
- The patient is well, in spite of the pathology that afflicts him.
Results
The best results are obtained when all the main requirements, described so far and necessary for the implementation of the treatment, are met. Despite this, it is still difficult for anyone to predict the effects of a bone marrow transplant, as each patient is a case in itself.



