Generality
Phalloplasty is the plastic surgery procedure for building, reconstructing or enlarging the penis.

A rather complex operation, phalloplasty can be used in the presence of congenital penile defects (eg micropenis, epispadias or hypospadias) or anatomical alterations of the penis, following traumatic events or the removal of a tumor; phalloplasty is also one of the surgical procedures proposed to women who want to change sex and become men.
Modern phalloplasty involves the removal of a skin flap from an area of the body that is usually hidden from view and the re-use of this skin flap in the construction, reconstruction or lengthening of the penis (this depends on the purpose of the procedure), and in the prolongation or remodeling of the urethra (even in this situation, everything depends on the purpose of the intervention).
Although it is safer than before and guarantees better results than a few decades ago, phalloplasty is still today an intervention characterized by a significant risk of failure and complications.
What is Phalloplasty?
Phalloplasty is a plastic surgery for the construction, reconstruction or enlargement of the penis.
Phalloplasty is a rather complex procedure, which in some circumstances requires the execution of several distinct operations.
Currently, phalloplasty is achievable through various surgical techniques, which are the result of the evolution and improvement of modern plastic surgery.
Did you know that ...
Phalloplasty aimed at enlarging the penis is more properly called phalloplasty of lengthening .
History of Phalloplasty
- The first ever intervention of phalloplasty - whose purpose was the reconstruction of a penis - dates back to 1936 ; it was a Russian surgeon named Nikolaj Bogoraz who made it .
- The first phalloplasty intervention aimed at changing sex from woman to man dates back to 1946 ; the author of this historic operation was New Zealand plastic surgeon Harold Gillies, while the patient was Michael Dillon .
Over time, plastic surgery has evolved and perfected; therefore, today, the current techniques for the implementation of phalloplasty are different and, of course, much more effective, than not only those exploited by Bogoraz and Gillies, but also those of a few decades ago.
Purpose
Phalloplasty is a surgical operation that aims at the realization of an aesthetically well-formed penis, of the right dimensions, functional to the passage of urine and, finally, endowed with tactile sensitivity and the capacity for erection (or something similar to an erection).
Indications
Phalloplasty is indicated at:
- Men with congenital penile defects, such as micropenis, hypospadias or epispadias .
- Micropene: it is the medical term that indicates the presence of a penis with dimensions clearly inferior to the normality standards.
In an adult man, in order to speak of micropenis, the erect penis must be shorter than 7 centimeters; in a newborn, instead, it must be shorter than 1.5 centimeters;
- Hypospadias: it is the medical term that defines the presence of a not perfectly developed urethra and whose urinary meatus (ie the opening for the escape of urine) does not reside on the tip of the penis glans, but in a point of the ventral fascia of the latter.
- Epispadia: is the medical word that describes the presence of a not perfectly developed urethra and whose urinary meatus does not reside on the tip of the glans, but in point of the dorsal fascia of the penis.
- Micropene: it is the medical term that indicates the presence of a penis with dimensions clearly inferior to the normality standards.
- Men victims of serious traumas in the genital area, which have profoundly altered the anatomy of the penis;

- Men who, due to a penile tumor, had to undergo the removal of a part of the organ affected by the tumor;
- Women who want to change sex and become full-fledged men ( transgender women ).
If in the first 3 circumstances (where the patient is a man) the phalloplasty corresponds to a work of reconstruction / enlargement of the penis (in any case it is an intervention on an already existing organ), in the last (where the patient is a woman) consists in a procedure for the construction of a new penis.
Two important notes on phalloplasty for sex change:
- The phalloplasty for sex change from woman to man is the specular intervention of vaginoplasty for the change of sex from man to woman.
- Phalloplasty for sex change should not be confused with metoidioplasty, which is a woman-to-man sex change surgery, preceded by a testosterone-based hormone therapy and characterized by the transformation of the clitoris into something of very similar to a penis.
Preparation
Before the phalloplasty, there are:
- A thorough medical examination, on the occasion of which the surgeon who performs the surgery knows the patient candidate, learns about problems and clinical history (eg: presence of allergies, medications taken, general health, presence of chronic diseases, etc.), and informs him of all the details of the intervention, in particular the rules to be scrupulously respected before the procedure, so that the latter takes place for the better;

- A series of diagnostic tests, such as blood tests, electrocardiograms, urine tests, etc., which serve to clarify the health status of the patient candidate and ascertain that the latter is fit to undergo surgery.
Pre-Operative Instructions: what are they?
Pre-operative instructions are those set of indications that a patient must have the foresight to follow, in the days preceding a certain surgical procedure.
In the case of phalloplasty, the pre-operative instructions consist of:
- Stop smoking (this makes sense, of course, if the patient is a smoker). Cigarette smoking increases the risk of surgical incisions becoming infected; moreover, it alters the flow of blood to the skin, which leads to a slowing down of the closure of the aforementioned incisions.
According to industry experts, smoking patients should initiate smoking cessation at least 2 weeks before surgery and implement it at least 2 weeks after the operation.
- Temporarily stop, starting from a few days before the phalloplasty, any drug therapy that alters the normal process of blood coagulation (therefore, suspend any treatments based on aspirin, warfarin, heparin etc.).
- On the day of the procedure, appear at full fast for at least 8 hours . This means that, if phalloplasty is expected in the morning, the last meal taken by the patient is the dinner the day before the operation.
Fasting is part of the pre-operative instructions of any surgical procedure that includes general anesthesia or that, in particular circumstances, could include general anesthesia.
- Ask a close relative or friend for support on the day of the procedure, especially with regards to returning home, once the operation is completed.
Procedure
By reserving information on the execution techniques to a separate section, phalloplasty provides, very briefly, the removal of a flap of skin, with its vessels and nerves, from an area of the body that is usually hidden from view and the king - use of this skin flap in the construction, reconstruction or lengthening of the penis, and in the prolongation or remodeling of the urethra.
The use of a flap of skin including blood vessels and nerves is extremely advantageous, because it ensures the presence of a blood circulation and a nervous sensitivity to the penis (both on the occasion of a construction and a reconstruction or an extension) the surgeon's task is to connect the vessels and nerves in the new transplant site).
The extent of the extraction (ie the size of the flap of skin to be re-used for the penis) depends on the purpose of the phalloplasty: if the latter has as its objective the construction ex novo of a penis, the skin flap to be withdrawn will be larger, compared to what happens for a phalloplasty aimed at reconstruction or lengthening.
How is Phalloplasty in Women: some more details
The ex novo construction of a penis (therefore the phalloplasty on a woman who wants to change sex) is a much more complex and articulated operation than the reconstruction or lengthening of the penis (therefore the phalloplasty on a man), for the following reasons:
- Before phalloplasty, women who want to change sex must undergo a long series of fundamental surgical operations to become men, such as: removal of large and small vaginal lips, removal of the vagina ( vaginectomy ), removal of the uterus ( hysterectomy ) and elimination of the ovaries ( oophorectomy );

- During phalloplasty on a woman, except in special cases, the surgeon must:
- Create a sufficiently long tubular structure that acts as a urethra ( urethroplasty ). This is explained by the fact that the female urethra is much shorter than the male urethra.
Urethroplasty is not an obligatory practice, in the sense that patients can still opt for maintaining the original urethra (in this case, they will continue to urinate from a sitting position);
- To realize, around the tubular structure that acts as a urethra, a second tubular structure, clearly larger, which has the appearance of a penile body . In this way, the surgeon reproduced a true penis, with the urethra inside it;
- Join the neo-urethra and the neo-body of the penis to the patient's genital site using appropriate sutures;
- Re-elaborate the innervation to the genital area, so that the neo-penis has nerve sensitivity;
- Create a structure that, seen from the outside, acts as a scrotum ( scrotoplasty ) and, if the patient wishes, testicular prostheses (fake testicles) to be inserted inside. Normally, for scrotoplasty, surgeons use the skin of the vaginal lips;
- To be able to count on a penis with erectile capacity, women subjected to phalloplasty must face a further surgical operation, aimed at positioning a penile prosthesis (it is a kind of pump that allows the erection of the neo-penis).
Some curiosities about phalloplasty for sex change
- The positioning of the penile prosthesis can only take place once the surgical wounds, practiced for phalloplasty, have completely healed; this procedure can therefore take place only a few months after the phalloplasty.
- Some surgeons prefer to "break" the phalloplasty into several procedures (eg: making the penis and urethra in an operation and creating the scrotum in another surgery).
Surgical techniques for performing a phalloplasty
To characterize a surgical technique for performing a phalloplasty is the site of the removal of the skin flap necessary for the operation.
Currently, there are 4 surgical techniques useful for making a phalloplasty:
- The technique that involves taking the flap of skin from the radial forearm ( phalloplasty with a radial flap of the forearm ). It is the most recent and most performed technique, as the skin flap of the radial forearm ensures a high sensitivity to the penis;

- The technique that involves taking the flap of skin from the latero-anterior portion of the thigh ( phalloplasty with a latero-anterior flap of the thigh ). It is an increasingly less used technique, as the latero-anterior thigh flap shows little nervous sensitivity;
- The technique that involves taking the flap of skin from the abdomen ( phalloplasty with an abdominal flap ). It is the ideal technique for female patients who renounce urethroplasty;
- The technique that involves the removal of the skin flap from the skin area that covers the large dorsal muscle or latissimus dorsi ( phalloplasty with a muscissocutaneous latissimus dorsi flap ). This technique is particularly useful when it is necessary to build a penis within which a penile prosthesis will be placed later.
After the Procedure
IMMEDIATELY AFTER THE FALLOPLASTY
In general, after phalloplasty, a one-day hospitalization period follows, for simpler operations, and 2-3 days, for more complex operations (such as, for example, sex change operations) .
During hospitalization, medical personnel take care of the patient, periodically monitoring their health conditions.
In some circumstances (eg phalloplasty due to the change of sex), the hospitalization also includes the insertion of a bladder catheter for the expulsion of urine, a catheter that the patient must maintain for 1-2 weeks.
AFTER THE HOSPITALITY
Upon returning home, the patient must be at rest from any physical activity for a period of time that can range from 4 to 8 weeks, depending on the complexity of the intervention to which he is subjected (eg: the phalloplasty for changing the sex involves a period of rest from physical activity much longer than that expected in the case of a reconstructive phalloplasty).
The first days following the operation are characterized by pain, bruising and burning during surgery, blood in the urine, nausea and lack of nervous sensitivity at the level of the operated organ; over time, however, these disorders vanish: pain, bruises, burning and nausea disappear, the urine no longer contains blood and the transplanted skin flap is sensitive to the touch.
To get the most out of phalloplasty, during the first few weeks following the operation, the patient must:
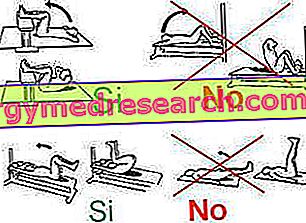
- Avoid applying pressure to the operated area;
- Try to keep the operated area high, to prevent it from swelling;
- Keep the operated area clean, according to the instructions of your doctor. Cleaning is essential to avoid infections;
- Do not apply ice;
- Avoid showering, unless otherwise advised by the doctor (personal cleaning of the operated area must take place in other ways, which the doctor will expose in the appropriate places);
- Empty the bag tied to the bladder catheter (if provided) at least 3 times a day;
- Do not pull the bladder catheter (if provided).
Did you know that ...
After a phalloplasty, the appearance of an appreciable nervous sensitivity at the level of the intervention zone could occur even after many weeks .
Risks and Complications
Thanks to the improvement of surgical techniques, today phalloplasty is a safer operation than in the past; nevertheless, however, it remains an intervention characterized by a risk of complications that is by no means negligible.
Risks of Phalloplasty: what are the Complications?
Phalloplasty presents the classic risks associated with any surgical procedure ( generic risks ), plus a series of risks characteristic of the same phalloplasty ( specific risks ).
Generic risks include:
- Excessive bleeding during surgery;
- Development of an infection at the surgical incision;
- Deep venous thrombosis;
- Adverse reaction to anesthetics;
- Formation of dangerous blood clots.
Specific risks include:
- Urethral fistula ;
- Urethral stricture ;
- Necrosis of the transplanted skin flap;
- Damage to the bladder or rectum ;
- Absence of nervous sensitivity .
The patients most at risk of complications are those subjected to phalloplasty due to the change of sex, therefore female patients, due to the complexity of the intervention.
Results
Thanks to the improvement of plastic surgery in recent decades, today, phalloplasty guarantees better results than before; despite this, however, there is still a surgical procedure characterized by a non-negligible percentage of failures and a real risk of complications.
Phalloplasty procedures with the highest probability of failure are those for sex change.