Generality
Sono-hysterography, also known as hysterosonography, is a transvaginal ultrasound that allows a fairly accurate analysis of the internal cavity of the uterus.
In general, doctors prescribe it when, based on a certain symptomatology or the patient's medical history, they suspect uterine-level problems such as: polyps, fibroids, congenital anomalies, malignant tumors, endometrial adhesions, etc.
Minimally invasive, non-hysterography does not require special preparation and consists of two consecutive major moments: the first, in which the doctor performs a simple transvaginal ultrasound to assess the orientation of the uterus, and a second, in which he analyzes in full the whole uterine cavity thanks to the injection of a specific saline solution.
The results are available immediately, but require the evaluation of a gynecologist.
Short reference to the uterus
Uneven and hollow, the uterus is the female genital organ that serves to receive the fertilized egg cell (that is, the future fetus) and to guarantee its correct development during the 9 months of pregnancy.

Figure: depiction of a normal uterus. According to the most accurate descriptions, the uterus presents two other areas, in addition to the body of the uterus and the uterine cervix: they are the isthmus of the uterus and the fundus (or base) of the uterus. The isthmus of the uterus is the narrowing that divides the body and the neck of the uterus. The fundus (or base of the uterus) is the upper portion of the body, located above the imaginary line that connects the two fallopian tubes. It is rounded in shape and protrudes forward.
It resides in the small pelvis, precisely between bladder (anteriorly), rectum (posteriorly), intestinal loops (superiorly) and vagina (inferiorly).
During the lifetime, the uterus changes its shape. If up to the prepubertal age it has an elongated appearance similar to a glove finger, in adulthood it looks a lot like an inverted (or upside down) pear, while in the post-menopausal phase it gradually reduces its volume and is crushed.
From a macroscopic point of view, doctors divide the uterus into two distinct main regions: a larger and larger portion, called the uterus body (or uterine body ), and a narrower portion, called the cervix (or cervix ). The uterine cervix protrudes, to a minimum extent, inside the vagina: it is the so-called "tench snout".
| Measurements and weight of the uterus in an adult woman | |
| Medium length | 7-8 centimeters |
| Transverse diameter | 4-5 centimeters |
| Antero-posterior diameter | 4 centimeters |
| Weight | 60-70 grams |
What is Sonohysterography?
Sono-hysterography, or hysterosonography, is an ultrasound that allows accurate study of the uterine cavity via the transvaginal route.
It is a minimally invasive diagnostic technique, in that - beyond the insertion into the vagina of the ultrasound probe - it does not foresee any exposure of the patient to radiation harmful to health.
ADDITIONAL PROCEDURES
Sono-hysterography could also include the study of blood flow in vessels that supply the uterus and other neighboring organs of the genital tract.
The ultrasound examinations that also allow an analysis of the blood supply are the so-called Doppler ultrasound scans .
HOW DOES AN ECOGRAPHY WORK?
The instrument with which the doctors carry out an ultrasound is the ultrasound system. An ultrasound system includes three main elements: a computerized console, a monitor and an ultrasonic probe (or transducer ).
The ultrasound probe is the element that, leaning against the body, allows the organs and tissues located inside the examined area to be displayed on the monitor (after processing by the computerized console).
The transducer works like this: thanks to the passage of alternating electric current, the probe produces a certain amount of ultrasound; these penetrate through the skin and affect the underlying tissues (or organs). A portion of penetrated ultrasounds is subject to refraction - that is, it is absorbed by the tissue - while another portion is subject to reflection - that is, it goes back to the transducer.
In striking the probe, the reflected altitude (also called echo) generates an electric current, which the computerized console can interpret and transform into images on the monitor.
The resolution of the images depends on the frequency of emission of the ultrasounds: the greater this frequency, the greater the penetration of the ultrasounds in the tissues and the better the resolution.
The ultrasound gel
As the readers who have undergone some kind of ultrasound examination in the past, the doctor applies a particular gel to the area of the body that he intends to examine with the probe.
Each type of ultrasound involves the use of this gel, as it is essential to eliminate the air that could interpose between the transducer and the anatomical area under examination.
All this allows for better quality images.
When you run
Doctors prescribe a sonohysterography when, based on some symptoms or signs present in a woman, they suspect some uterine problem, including:
- Polyps
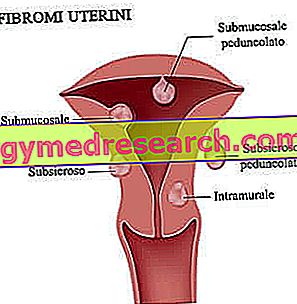
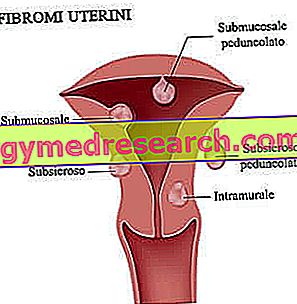
- fibroids
- Endometrial atrophy
- Endometrial adhesions
- Malignant masses or tumor lesions
- Congenital defects.
Furthermore, they also resort to them when they have to investigate cases of infertility or continuous miscarriages .
SONO HYSTEROGRAPHY DOPPLER
Doppler hysterography allows the doctor to evaluate:
- The presence of any obstacles along the blood vessels; obstacles, such as a clot, which prevents normal blood flow.
- Blood flow in polyps, fibroids and congenital malformations.
- The presence of pelvic varicose veins (also known as pelvic varicocele) or aneurysms.
WHEN IS IT CONTRAINDICATED?
Sono-hysterography is contraindicated in at least two situations:
- In case of pregnancy . In light of this, women who suspect they are even minimally pregnant should notify their gynecologist, who can make the most correct decisions.
- In the case of pelvic inflammatory disease . It is an inflammatory process, of an acute or chronic nature, which affects the female reproductive organs and adjacent structures. The most affected structures are the fallopian tubes; then followed by the uterus, the ovaries and the pelvic peritoneum. Some infectious agents, such as Chlamydia trachomatis, Neisseria gonorrhoeae and Mycoplasma hominis, generally cause it.
FOLLOW UP
Some pathologies and abnormalities of the uterus require periodic monitoring, especially during treatment or recovery from surgery (at the uterus).
This monitoring includes a series of diagnostic tests, often including the hysterography.
Preparation
Sonoysterography requires no special preparation. Therefore, it is not necessary to go on an empty stomach, interrupt any pharmacological treatment, etc.
The only advice that doctors give is to wear comfortable clothing.
WHAT IS THE BEST MOMENT FOR TAKING THE EXAM?
According to the medical opinion, the best time to undergo sonoysterography is the first week after menstruation . The reasons for this are at least two:
- Immediately after menstruation, the endometrial mucosa is very thin, which makes it much easier to visualize the uterine cavity.
- It is almost certain that the patient is not already pregnant.
However, it should be noted that this timing is generally valid. In fact, in some special circumstances (NB: it depends on the symptoms), doctors prefer to conduct the examination at other times in the menstrual cycle, because it is more useful for the purposes of obtaining information.
IN THE DAY OF THE PRECEDURA
Patients must empty their bladder shortly before performing hysterography.
Procedure
Once the patient has been seated on a classic gynecological table, the radiologist (or a competent medical technician) initiates the sono-hysterography with a simple transvaginal ultrasound, in order to first evaluate the orientation of the uterus and the appearance of the ovaries. For this first analysis, apply a sterile envelope and the classic ultrasound gel (NB: in this situation, it also acts as a lubricant).
At the end of the transvaginal ultrasound, it extracts the probe and inserts a sterile speculum into the vagina.

Once the saline solution has been injected, the speculum is extracted and the ultrasound probe is inserted again, this time to accurately visualize the internal cavity of the uterus.
During Doppler hysterography, the ultrasound probes used and the access route remain unchanged. What changes is the image observed on the monitor, which shows different colors depending on the blood flow.
HOW LONG IS THE PROCEDURE?
The procedure described above lasts between 20 and 30 minutes.
WHAT DOES THE PATIENT DURING THE EXAM?
Sono-hysterography is a generally painless exam. In fact, the cases of women who find it annoying or not very tolerable are very rare and do not depend on how serious the symptoms are (this means that very pronounced symptoms do not affect the tolerability of the procedure).
Sometimes, the exam can cause small cramps and brief episodes of vaginal bleeding.
The former are due to the saline solution used; the latter last a few days and are a normal consequence of the insertion of the speculum and the probe in the vagina.
AFTER THE PROCEDURE
Since non-hysterography does not involve the administration of anesthetics or sedatives, at the end of the examination the patients can return home immediately and immediately engage in normal daily activities.
Risks, advantages and limits
Sono-hysterography is a diagnostic procedure with almost no risk, as it does not involve injections, incisions or drug administration with possible serious side effects.
ADVANTAGES
Some advantages, such as minimal invasiveness, high tolerability and non-use of ionizing radiation harmful to health, has already been discussed. However, hysterosonography has other points in his favor:
- It is available to most, as it is not as expensive as other diagnostic imaging procedures.
- The images of the soft tissues provided are clear, much more than those obtained with some X-ray examinations (which are harmful ionizing radiation).
- It is of relatively short duration.
- It allows us to identify uterine anomalies that normal transvaginal ultrasound scans (ie those in which the distension of the uterine walls is not foreseen) are not able to capture.
- It allows to establish if a certain condition of the uterus (for example, polyps or fibroids) is severe to the point of requiring surgery. In other words, it clarifies when it is appropriate to operate and when it is not.
LIMITATIONS OF THE PROCEDURE
The limits of sonohysterography emerge on a few occasions.
One of these is when patients have a stenosis of the cervix (NB: stenosis is the medical term for pathological narrowing). This condition does not allow the insertion of the catheter for the injection of the physiological saline solution, the purpose of which is to stretch the walls of the uterus. As will be recalled, the enlargement of the uterine cavity plays a fundamental role in obtaining clear and meaningful images.
Results
Very often, the results of the hysterography are available to the patient at the end of the procedure. To put the result in writing is always a medical radiologist, who observes and evaluates the images processed by the ultrasound.
At this point, it is essential and necessary to consult your trusted gynecologist, who will express an opinion on what emerged from the hysterography and plan a possible treatment.