Generality
The papilledema (or edema of the optic papilla) is the swelling of the optic disc, that is the portion of the retinal plane that corresponds to the origin of the optic nerve (the pair of cranial nerves). At this level, in fact, the axons of about one million ganglion cells of the retina converge, about to exit the eyeball to head towards the diencephalic level. In other words, the optic disk represents the beginning of the nerve pathways involved in vision, capable of transmitting information from the retina to the visual cortex.
Papilloedema in the strict sense is caused by the increase in pressure inside the brain (intracranial hypertension) and can be associated with trauma, tumors, abscesses or cerebral haemorrhages. Unfortunately, this pathological event does not cause early symptoms, although the vision may be transiently disturbed.
The diagnosis is made through ophthalmoscopy, followed by further tests, usually neuroradiological, aimed at identifying the cause.
The therapy is directed at the underlying disease and must be set up as soon as possible in order to avoid permanent outcomes of the visual apparatus or worse secondary consequences to intracranial hypertension.
Optical papilla: what is it?
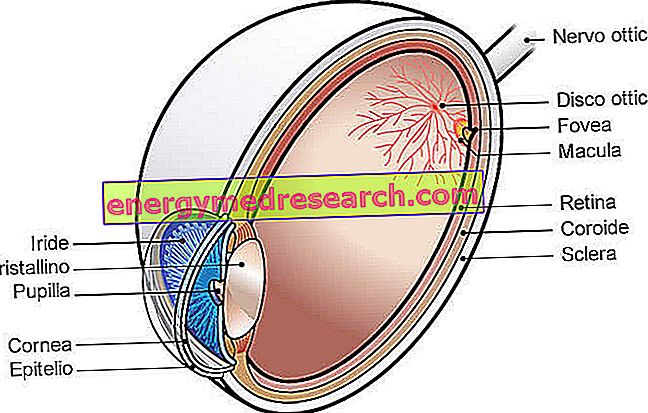
The optic papilla (or optic disc) is a small oval area of the retinal plane, with a diameter of 1.5-2 mm and a whitish color. Lying low and medially with respect to the posterior pole of the eye, nasally with respect to the macula, this area has well delimited margins and a flat or excavated surface in the center.
The optic papilla is the only blind area of the retina, as it has no photoreceptors.
From the center of the optic disc, the blood vessels that supply the eye emerge.
Pathogenesis
The edema of the optic papilla secondary to intracranial hypertension is almost always bilateral, so both optic nerves appear swollen.
The appearance of this sign depends on the increase in pressure in the area between the arachnoid meninges and the pia mater that surround the optic nerve, communicating with the endocranial subarachnoid space and filled with cerebrospinal fluid (also called liquor or cerebrospinal fluid). The increase in intracranial pressure, therefore, is transmitted through the liquor also inside the sheath of the optic nerve, causing a compression around the same and a swelling of the axons posterior to the optic papilla. This phenomenon also hinders venous return via the central vein of the retina, which runs inside the optic nerve and drains the blood from the eye.
In the initial phase, the optic papilla is hyperemic and without normal physiological excavation; the margins swell, rising again on the retinal plane, and become more blurred. Subsequently, the venous stasis of the papillary veins appears, which appear congested and may undergo frequent bleeding.
In the more advanced stages, the optic papilla may undergo atrophy, a condition that involves the degeneration of the optic nerve and the onset of severe visual disturbances.
Causes
Papilledema is a sign of increased intracranial pressure.
The causes include:
- Primary or secondary brain tumor;
- Brain abscess;
- Head trauma;
- Cerebral hemorrhage;
- Meningitis;
- Encephalitis;
- Arachnoid adhesions;
- Cavernous or dural sinus thrombosis;
- Pseudotumor cerebri (idiopathic endocranial hypertension).
Symptoms
Initially, edema of the optic papilla does not compromise vision: in general, visual acuity and pupillary reflex to light are normal. In later stages, however, visual blurs, intermittent scotomas, visual field defects and diplopia appear. In addition, patients may exhibit symptoms due to increased intracranial pressure: jet vomiting, headache, tinnitus, paresthesia and alterations in consciousness.
A sharp decrease in visual capacity, on the other hand, occurs with the onset of progressive optic atrophy, which is preceded by episodes of fleeting amaurosis (transient blindness).
Diagnosis
The clinical evaluation of papilledema begins with the observation of the fundus through the ophthalmoscope. This examination reveals congested and tortuous retinal veins and an hyperemic optic papilla, with shaded contours. On ophthalmoscopic examination, furthermore, bleeding can be found in papillary and peripapillary areas, but not in the retinal periphery.
Ophthalmoscopy can provide a finding analogous to that of the papillary infarct of the optic nerve, papillitis or intraorbital optic neuritis, therefore the outcome of the investigation must necessarily be integrated with medical history, examination of visual function and neuroimaging investigations. Examination of the visual field can detect an enlargement of the blind spot of the eye.
If there is a clinical suspicion of papilledema, an MRI with gadolinium or a computed tomography (CT) with contrast medium should be performed immediately. These tests are necessary to rule out the presence of an intracranial mass. Once the presence of an intracranial space-occupying lesion is excluded, it is necessary to perform lumbar puncture and the measurement of the cerebrospinal fluid (LCR) pressure.
Differential diagnosis
The term " papilledema " must be reserved, in the strict sense, for the swelling of the optic disc referred to an increase in intracranial pressure. An isolated swelling of the optic papilla without liquor hypertension (caused, for example, by an optic neuritis or an ischemic optic neuropathy) is instead indicated simply as " optic disc edema ".
The swelling of the optic papilla, in fact, is also found in other pathological processes. In particular, it can result from inflammation (including optic neuritis, uveitis and papillitis), vascular events (arterial hypertension, ischemia, thrombosis and blood vessel obstruction), trauma, infectious infiltration, orbital and intraocular tumors, hereditary factors (pseudo-papillitis ) and toxicity from drugs or exogenous agents (eg arsenic and inorganic lead poisonings).
The differential diagnosis requires a thorough ophthalmological evaluation. The papilledema secondary to intracranial hypertension is typically bilateral. Optic disc edema, on the other hand, is often unilateral and involves early visual disturbances and alterations of the chromatic sense.
Treatment
Treatment must be set up as soon as possible. The type of therapeutic intervention depends on the etiology of papilledema and has the aim of reducing intracranial pressure.
If this is not restored to normal values, in fact, an atrophy of the optic nerve may occur. This complication leads to a severe reduction in the visual capacity associated with other serious neurological sequelae.



