Complications of lichen planus
Some hypotheses have been formulated regarding the dangers that could derive from the dermatosis of lichen planus: some affected patients could be at risk of tumors of the skin, penis, oral mucosa and vulvovaginitis. In this regard it is advisable to seek medical attention from the earliest cutaneous manifestations, to ascertain that the disease does not degenerate into carcinoma.
Diagnosis
As we have already analyzed, the reticular lesions of lichen planus are almost unmistakable, therefore the diagnosis is quite simple. Unfortunately, for the other forms of lichen, recognition does not appear so easy, therefore, when the patient is not subjected to a correct diagnostic investigation, there is the risk of confusing lichen for more simplistic diseases.
In general, the doctor hypothesizes a first diagnosis based on the symptoms complained of by the patient, then proceeds with a dermatological examination and possibly with laboratory tests, such as allergy examination, hepatitis C test and incisional biopsy, thus researching the possible etiological elements responsible for lichen planus.
therapies
To learn more: Drugs to treat Lichen Planus
Lichen planus is a subtle and equivocal disease, in which the therapy is almost problematic: in some subjects the dermatosis could last for long periods, in others it could even heal spontaneously. It is necessary to pay more attention to the lichen planus of the scalp, genitals, mucous membranes and nails, guilty of being the most harmful in terms of symptoms: in fact, the lichen planus that affects these areas tends to last a long time, besides generating significant and annoying inconveniences.
Inflammation is generally treated with topical corticosteroids (applied directly in situ), administered orally or injected intravenously. From a therapeutic point of view, cortisone derivatives are extraordinary because they are very effective, but on the other hand, they are easily responsible for complications such as, for example, irreversible epithelial atrophy and oral candidiasis. Furthermore, the excessive use of oral and intravenous cortisone can cause diabetes mellitus, osteoporosis and hypercholesterolemia.
In addition to these drugs, according to the type of lichen planus and the symptoms, the doctor can also prescribe retinoids (whose use must be banned during pregnancy, because teratogens), antihistamines and phototherapy (UVB).
Sometimes, drugs with an immunosuppressive action are prescribed, such as cyclosporine, particularly effective in the case of erosive lichen; even this pharmaceutical specialty is not without side effects, as it could generate toxicity in the kidneys.
Unfortunately, most patients are destined not to heal at all and are forced to live with lichen planus throughout their lives, since the etiological factor that is really (and not only ideally) responsible for dermatosis is still unclear: once diagnosed, the patient must scrupulously follow the therapeutic treatment for life.
Summary
Lichen planus in brief:
| Disease | Lichen planus |
| Description | Chronic inflammatory dermatosis deriving from immunology, which mainly involves the skin, mucous membranes and nails |
| Imprint of recognition of the disease | Pruritic and Purple Polygonal Papules (4P disease) |
| Course | Relapsing, benign in nature |
| Etymology of the term | The term derives from the typical manifestations of the disease, very similar to the arborescent formations of lichens |
| Incidence of lichen planus | Lichen planus:
|
| Etiology of lichen planus | Uncertain; the possible triggers are:
|
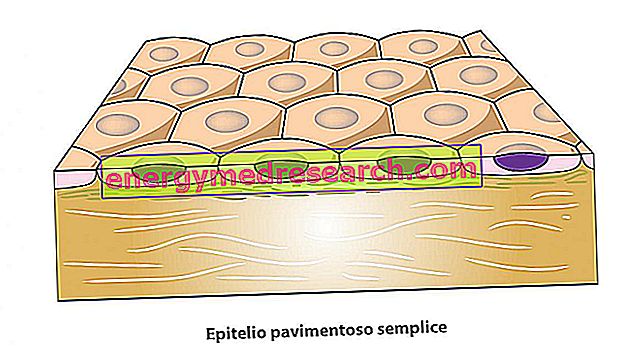
| Histopathology | Alteration of the cellular composition of the injured anatomical sites:
|
| Classification |
atrophic lichen reticular lichen erosive lichen (ulcerative or atrophic) plaque lichen planus
|
| Complications of lichen planus | Risk of tumors of the skin, penis, oral mucosa and vulvovaginitis |
| Lichen planus diagnosis |
|
| Therapies against lichen planus |
The patient suffering from lichen planus must strictly follow the therapeutic treatment for life. |