Genes involved in schizophrenia
Currently the genes involved in schizophrenia are COMT (cathecol-O-methyltransferase; NRG1 (neuregulin 1) and DISC 1 (disrupted in schizophrenia 1). Some of the main features related to the genes involved will be briefly explained.
- COMT is the gene that codes for an enzyme that degrades catecholamines. It is expressed in high concentrations in the prefrontal cortex and in the hippocampus, more specifically in the extra-synaptic space. Since at the level of the prefrontal cortex the transporters for the dopamine neurotransmitter are few, it has been hypothesized that COMT has the function of compensating the dopamine in the prefrontal cortex. Some studies have also shown that a single nucleotide polymorphism on the COMT gene causes a reduction in enzyme activity in the brain and lymphocytes. This decrease in enzyme activity results in a higher level of dopamine in the prefrontal cortex.
- NRG1 and its ERB4 receptor play a very important role during the development of the central nervous system. In particular they seem to be important for the form of GABAergic interneurons that contain parvalbumin. Not only that, in the post-natal period, it has been seen that NRG1 plays an important role for plasticity in glutamatergic synapses and is also involved in the differentiation of oligodendrocytes.
- DISC1 is an anchoring protein with multiple functions. It is involved in processes such as proliferation of neural progenitors, differentiation and dendritic arborization. At the level of the prefrontal cortex, it influences verbal fluidity.
Abnormalities of the central nervous system
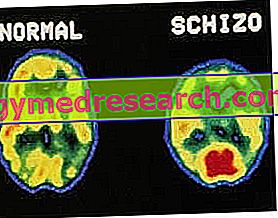
Along with the genetic alterations described, it has also been observed that at the cerebral level individuals affected by schizophrenia have alterations in their structure and functioning.
- Pyramidal neurons represent about 75% of the neurons in the cortex. They are neurons that use glutamate, an excitatory neurotransmitter, important for the correct execution of cognitive functions. Numerous studies have shown the presence of anatomical alterations at the level of these neurons; for example, schizophrenic patients had a reduction in dendritic spines, shorter dendrites and poor arborization compared to a healthy subject. This has led to the hypothesis that the individual affected by schizophrenia has a reduction in excitatory inputs, and therefore an alteration in the glutamate system level.
- GABAergic interneurons, which use GABA, an inhibitory neurotransmitter, account for about 25% of cortex neurons. They regulate the activity of pyramidal neurons. It is now known that in schizophrenia there is an alteration of GABAergic inhibitory neurons in the cortex. In particular, a reduction in the levels of GAD67 is documented, the main enzyme that synthesizes GABA.
- The axons that originate from neurons of the thalamus and from dopaminergic neurons in the midbrain, modulate the activity of pyramidal neurons and of GABAergic interneurons. It has been shown that schizophrenic individuals show a reduction in the dopaminergic signal that could be due to either a reduction in the number of axons or a reduced synthesis of dopamine. It has also been hypothesized that the reduced availability of dopamine may depend on an alteration at the COMT gene level, responsible for dopamine levels in the cortex.
Since the deficits related to working memory seem to be a peculiar feature of the pathology in question, it is logical that trying to understand the nature of the alterations affecting the neuronal circuitry in the cortex may be useful for the identification of new molecules targets.
Recently, in addition to the classic neurotransmitter systems mentioned above, it has been shown that other signaling systems can also be altered in schizophrenia. Among these, the chinurenine pathway, responsible for the synthesis of quinurene acid, seems to play an important role. Indeed, quinurene acid has been shown to be present in high concentrations in the brains of individuals with schizophrenia.
Quinurene acid
Quinurene acid is a product that derives from the metabolism of the amino acid tryptophan, has a neuroinhibitory action in the central nervous system and is implicated in some neurodegenerative diseases. Numerous studies suggest that drugs capable of reducing the high levels of quinurenic acid found in the brains of schizophrenic patients, could be combined with the current antipsychotic treatment regimen, to treat cognitive disorders of this disorder. Indeed, it has been shown that antipsychotics are able to act towards positive symptoms such as hallucinations and delusions, but are not able to act on cognitive deficit. There are many hopes for this new therapeutic strategy which involves quinurene acid. In fact there are studies conducted on animal models in which cognitive abilities were tested following treatment with quinurene acid. From these studies it emerged that only 28% of the animals in which chinurenic acid overproduction had been induced, had failed to solve problems that the control animals solved easily.



