Generality
Cervical cancer is one of the most common malignancies affecting the female genital tract. The pathological process involves, in particular, the uterine cervix, ie the lower portion of the uterus.

Often, in the early stages, cervical cancer does not cause signs or symptoms. However, the disease is characterized by slow evolution, which makes it curable if diagnosed early. For this reason, it is important to regularly undergo gynecological checks and screening tests (such as the Pap test or HPV test), useful for identifying precancerous lesions and intervening before they evolve into carcinoma.
Treatments for cervical cancer include surgery and radiation therapy, sometimes in association with chemotherapy .
Anatomy outline
- The cervix (also called the neck or portio) is the lower part of the uterus, a hollow, pear-shaped organ, located in the female pelvis, between the bladder (anteriorly) and the rectum (posteriorly).
- The uterine cervix is in direct connection with the vagina and is visible at the gynecological inspection as a cylindrical formation that presents an orifice in the center. The latter represents the extremity of the cervical canal, which connects the uterine cavity to the vagina.
- The cells that line the cervix are not all the same: the ectocervice is lined by squamous cells (like the vagina), while the endocervix (closer to the body of the uterus) has a glandular columnar epithelium. In the transition zone between these two cell types, called squamo-columnar junction, most of the cervical cancers originate.

Causes and risk factors
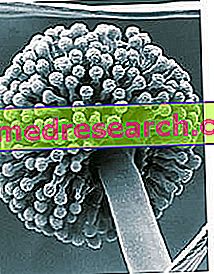
Cervical cancer is the first tumor for which an infectious cause has been recognized. The responsible micro-organism is the human papilloma virus (HPV), a viral agent that is widespread in the population, which is transmitted mainly through sexual contact.
The cervical cancer is caused, in particular, by the infection of some types of HPV, mainly strains 16 and 18, implicated in most cases (about 70%) and also involved in the onset of other neoplastic diseases of the female and male genital sphere, of the anus and oral cavity.
HPV infection is usually asymptomatic, so those affected do not know they are, greatly increasing the risk of virus transmission; it is estimated that about 75% of women have contracted it at least once in their life.
In most cases, HPV infection is completely overcome by our body, over a period of several months, without affecting health. However, when the virus is not eliminated by the immune system, the infection persists and promotes the onset of cellular abnormalities in the genital area; therefore, numerous pathologies can develop, benign and malignant, which affect women and men .
The tumor is preceded by precancerous changes in the tissue that covers the cervix ( dysplasia ). Some of these can regress spontaneously or remain unchanged; a small percentage of dysplasias may evolve, instead, into a real tumor, especially in the presence of some cofactors (such as states of immunodepression or active smoking).
In general, the time between infection and the onset of precancerous lesions ( cervical intraepithelial neoplasia or CIN ) is approximately 5 years; before the actual cervical cancer develops, however, 10-15 years may pass.
These long times make it possible to effectively implement the screening programs (Pap test and HPV-DNA test) and to have excellent results in terms of prevention.
Note. There are over 100 types of human papilloma virus: some of them are responsible for benign lesions, such as warts (HPV 6 and 11); others are capable of producing precancerous lesions (dysplasias) which, if left untreated, can become invasive, evolving into cervical cancer (species HPV 16 and HPV 18, considered "high-risk" oncogenes, that is strongly associated with neoplasia) ).
Human papilloma virus (HPV) infection is a necessary but not sufficient cause for cervical cancer development.
Other factors that can increase the risk of disease are:
- Lack of regular medical / gynecological control;
- Tendency to have numerous sexual partners;
- Tobacco smoke;
- Use of long-term oral contraceptives (for more than ten years);
- Sexually transmitted infections, in particular from Chlamydia trachomatis or herpes simplex type 2 virus (genital herpes);
- Family arrangement;
- High number of pregnancies;
- States of immunodepression.
Cervical cancer can affect all women, regardless of age, therefore, not only the most mature ones. A girl who becomes sexually active early has a greater risk of contracting human papilloma virus infection.
The age at risk for the infection begins, therefore, at the beginning of sexual activity and, based on the estimates, reaches its peak between 20 and 25 years.
Epidemiology
- Cervical cancer is one of the most frequent gynecological cancers worldwide.
- In Europe, it is the second leading cause of death from carcinoma (after breast cancer) in women under the age of 40. However, the number of deaths associated with the disease continues to decline, mainly due to the introduction of screening tests.
- In Italy, around 3, 500 new cases are estimated each year for cervical cancer.
Types
Cervical tumors are classified according to the cells from which they originate and are mainly of two types:
- Squamo-cell carcinoma : is the most frequent form (80% of tumors). It develops from the squamous cells that line the surface of the exocervix; it mainly affects women between 20 and 40 years old.
- Adenocarcinoma : less frequent (about 15% of cases), derives from the transformation of glandular cells of the endocervix.
Less common (3-5% of cervical tumors) are cervical tumors that present a mixed origin ( adenosquamous carcinomas ).
Signs and symptoms
Most often, cervical cancer does not cause symptoms in the early stages of development; however, early signs of HPV infection can be identified by regular gynecological examinations. This also allows to adequately treat and resolve the initial tissue abnormalities, before they degenerate.
On the other hand, when a tumor develops, abnormal cervical cells become cancerous and invasive, they grow to form a bulky mass inside the cervix or invade surrounding tissues.
In general, the first warning signs are:
- Pain in the pelvic area or at the lumbar level;
- Abnormal vaginal bleeding (especially after sexual intercourse, in the interval between two periods or in a woman in menopause);
- Increased vaginal secretions (sometimes smelly).
In the most advanced stages, symptoms may occur due to tumor growth and the involvement of adjacent organs:
- Blood in the urine;
- Pain in the bones and back;
- Edema of the lower limbs due to lymphatic obstruction of the venous system;
- Loss of appetite and weight;
- Constipation;
- Obstructive Uropathy;
- Fatigue.
Diagnosis
Often, precancerous lesions affecting the cervix do not cause manifestations and are generally identified with regular gynecological checks and screening programs, aimed at healthy women in the absence of symptoms.
When the Pap smear shows no lesions, the exam has a negative result and the woman is invited to repeat the exam after three years; if the investigation is positive, instead, it means that the cytological examination has found the presence of abnormal cells.
In the latter case, in-depth diagnostic examinations are scheduled:
- Colposcopy : the gynecologist uses a special instrument, called a colposcope, which allows you to lighten the cervix and see it enlarged. In this way, it is able to confirm the presence of lesions, evaluate its extension and perform a biopsy examination.
- Biopsy : consists of a small tissue collection from the cervix, to be subjected to histological examination.
- Magnetic resonance and computed tomography : they are used to assess whether and how much the tumor is extended.
Treatment
The most appropriate therapeutic path is established above all based on the stage of cervical cancer.
Depending on the case, interventions may include:
Surgery
This approach is aimed at removing the abnormal tissue from the cervix or from regions close to it. The choice of the type of intervention to be performed therefore depends on the extent of the tumor.
When the tumor is in an early stage and localized only on the surface of the cervix, the surgeon may decide to remove the cancer cells with a method similar to that used to treat precancerous lesions (cold-blade or laser conization ). If the disease has invaded the deep layers of the cervix, but is confined and has not extended to the immediately surrounding parts, it is possible to eliminate the tumor, but leave the uterus and ovaries in place. In other cases, however, it may be necessary to surgically remove the entire uterus ( hysterectomy ).
Based on the spread of the disease (therefore based on the clinical stage), the removal of regional lymph nodes (pelvic and / or lumbo-aortic) may also be indicated to check for possible neoplastic involvement.
Tumors extended to adjacent organs (bladder and rectum) are usually treated with radio-chemotherapy protocols and very rarely, in selected situations, with radical surgical procedures .
Chemotherapy
This systemic treatment can be applied on its own (when cancer cells have spread to other organs) or in combination with radiotherapy or surgery.
Chemotherapy uses drugs usually given intravenously to destroy cancer cells. The side effects mainly depend on which agents are used and include: hair loss, poor appetite, nausea and vomiting, diarrhea and predisposition to bruising.
Radiotherapy
This therapeutic intervention uses high-energy rays to damage cancer cells and block their growth; stands out in external beam radiotherapy and brachytherapy . In the first option, ionizing radiation is administered from the outside; therefore the pelvic region containing the structures to be treated radiates. On the other hand, brachytherapy involves placing radioactive material directly inside the vaginal canal, so as to selectively hit the area affected by the tumor, without affecting the bladder and the rectum (thus reducing side effects). The procedure integrates external beam radiotherapy or is used in the completion of post-operative treatment.
Prevention
Cervical cancer can be effectively prevented both through early diagnosis and adherence to screening programs, and by vaccination against HPV .
The cytological analysis of the cervical tissue ( Pap test ) is able to reduce the mortality for this tumor up to 80%, while the HPV-DNA test, which identifies the possible presence of the virus, revealing a situation of increased risk to develop a precancerous, it allows to identify the disease in very early stages.
PAP test
The Pap test (or Papanikolaou test) is a useful exam for early identification of possible HPV injuries; for this reason, it is used in screening for cervical cancer. Cytological analysis of cervical tissue is recommended from the age of 25 and should be performed regularly by all women (even asymptomatic), once every three years.
The Pap test is quite simple: rubbing a special spatula and a swab, the gynecologist gently picks up some cells from the most superficial layers of the cervix and cervical canal. The sample thus collected is then crawled on a slide, sprinkled with reagent and sent to the laboratory.
Microscopic analysis of the sample makes it possible to identify any cells with precancerous or tumor characteristics and, based on their degree of atypicality, to estimate the level of tissue damage.
HPV-DNA test
The HPV test (or HPV-DNA test) allows the detection of the presence of papilloma virus DNA in cervical cells. Therefore, compared to the Pap test, it turns out that the woman has contracted a potentially oncogenic virus, even before any lesions develop.
The HPV test is carried out in a manner similar to that of the Pap test. A small amount of cells taken from the cervix is subjected to a laboratory test to find the virus, with certain advantages in terms of sensitivity.
However, a positive HPV-DNA test should not cause anxiety, as it does not necessarily mean that a tumor is present or that it will develop in the future; the exam is able to identify, in fact, even infections that could regress spontaneously. For this reason, HPV testing is generally recommended for women over 30-35 years
Vaccination
Some HPV infections can be prevented with the bivalent vaccine (against the HPV strains 16 and 18) or quadrivalent (against the HPV strains 16, 18, 6 and 11); recently a novel vaccine has also been proposed which also provides protection from genital warts.
The protocol includes three injections over a six-month period, administered by a doctor, nurse or healthcare professional. For the vaccine to be effective, it is important to complete the entire vaccination course. Moreover, the protective effect is greater if given at a young age, before the start of sexual relations, since the chances of having already come into contact with the virus are low.
For this reason, in Italy, the National Health Service recommends and offers free vaccination for girls who are 11 years old (in some regions, free admission is maintained up to 18 years, while others have extended the program also to young men ). Older people, on the other hand, can access HPV vaccination at a discounted price.
In any case, it is necessary to continue to undergo regular gynecological checks and screening.