What is Prostate Cancer
Prostate cancer is the most common male cancer; just think that in Italy, every year, about 42, 800 cases are diagnosed.
Prostate cancer affects mainly after 50 years. Cancer cells are present in about 40% of fifty-year-olds and the risk increases with age. Indeed, according to recent medical studies and statistics, almost all men over the age of 80 have a small outbreak of prostate cancer.
Data in hand, it is estimated that every Italian over 65 has a 3% chance of dying from prostate cancer. For this reason, it is good not to let your guard down: intervening in time means more chances to eradicate or contain the disease.
The prostate
The prostate is a roundish gland, similar to a chestnut, which belongs to the male reproductive system; it is placed in the pelvis (lower part of the abdomen), just below the bladder and in front of the rectum, surrounding the first portion of the urethra.

The main function of the prostate consists in helping to produce sperm, since it secretes part of the seminal fluid released during ejaculation (note: the seminal fluid together with the spermatozoa constitutes the sperm).
Symptoms
To learn more: Symptoms Prostate cancer
In the early stages, prostate cancer is often asymptomatic; this means that the patient does not feel any symptoms, remaining unaware of the condition. In recent years, thanks to the growing awareness of the dangers of the disease, most prostate cancers are diagnosed in these early stages. A urological examination accompanied to the control of the PSA (prostate specific antigen), by blood analysis, allows to identify the subjects at risk in which to carry out further tests.
If the tumor is ignored, the increase in its size is associated with problems associated with urination, as the organ surrounds the prostatic urethra. The changes within the gland, therefore, directly influence urinary function. Symptoms of prostate cancer may include:
- Difficulty urinating (hesitation);
- Frequent stimulation to urinate, especially at night (nocturia);
- Difficulty in maintaining a constant flow of urine (the flow is weak, intermittent or the feeling of not being able to completely empty the bladder persists);
- Pain or burning during urination;
- Blood in urine or sperm;
- Erectile dysfunction (impotence);
- Painful ejaculation;
- Discomfort in the pelvic area;
- Fatigue, loss of appetite and general malaise;
- Generalized pain in the back, hips or pelvis.
PLEASE NOTE: The described urinary symptoms manifest themselves in a similar way to other benign prostatic problems, such as prostatic hyperplasia (BPH) . For this reason, if one or more of these manifestations occur, it is advisable to undergo specific medical tests without panicking; it could indeed be a "simple" benign enlargement of the prostate. Furthermore, the appearance of these symptoms in acute form could be a sign of an inflammation of the prostate, generally bacterial: prostatitis .
A malignant prostate tumor can metastasize to the pelvic lymph nodes and progressively spread to other parts of the body. Prostate cancer tends to metastasize mainly to the bones of the spine, pelvis, ribs and femur. Bone pain, therefore, can be a symptom of advanced prostate cancer. If the metastasis compresses the spinal cord, it can cause weakness or numbness in the lower limbs, urinary and fecal incontinence.
Prostate cancer? Take the test and find out if you are at risk
Benign prostatic problems
Benign prostatic diseases are more common than neoplasms, especially after the age of 50; often, these conditions cause symptoms that could be confused with those of the tumor.
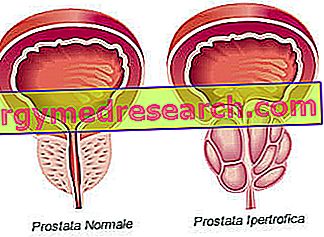
Under normal conditions, the prostate has the size of a walnut, but due to advancing age, or some pathologies, it can swell and determine the onset of disorders, especially urinary disorders.
Enlarged prostate (benign prostatic hyperplasia). The prostate is very sensitive to the action of hormones, such as testosterone. Over the years, an enlargement of the gland occurs spontaneously, following the hormonal changes that occur in the testicle (androgen production decreases and the release of small amounts of estrogen hormones begins). Benign prostatic hyperplasia can compress the urethra and create problems in the passage of urine.
Inflammation (prostatitis). Prostatitis is an inflammation of the prostate. Usually, the main cause is a bacterial infection, but it can also arise in the absence of pathogens. The symptoms consist of lower abdominal pain, often accompanied by dysuria, and loss of mucous secretions.
Precancerous lesions
Some precancerous conditions have the potential to evolve into prostate cancer, although this has yet to be established with certainty:
- Prostatic intraepithelial neoplasia (PIN) : under the microscope, the cells of the prostate gland are characterized by small alterations in shape and size, which make them abnormal. Many men may present with mild dysplasia (PIN1, low grade) even at a young age, but they will not necessarily develop prostate cancer. A high grade prostatic intraepithelial neoplasm, on the other hand, correlates to a significantly greater risk. For this reason, doctors must carefully monitor each patient in which they are found and, if necessary, perform another prostate biopsy.
- Proliferative inflammatory atrophy (PIA) : prostate cells seem smaller than normal and there are no signs of inflammation in the area. Researchers believe that the lesion may evolve to high grade PIN or directly to tumor.
- Atypical microacinic proliferation (ASAP) : in this case, the outcome of the biopsy is uncertain, ie the prognostic meaning is not related to a specific nature of benignity or malignancy; for this reason, the patient is advised to repeat the biopsy after three months.
Benign and malignant tumors
In the prostate there are different types of cells, each of which can undergo a neoplastic transformation. However, the diagnosed tumors derive mostly from the inside of the gland and are classified as adenocarcinomas (or glandular carcinomas) .
An adenocarcinoma originates when the normal cells, constituting one of the secretory glands, become cancerous. During the initial stages, the lesions remain confined. Over time, the neoplastic cells begin to multiply and spread in the surrounding tissue (stroma), forming a tumor mass. This causes a swelling of the prostate surface, found during palpation of the gland through the rectal wall. In more advanced stages, the tumor can increase its size and invade neighboring organs, such as the seminal vesicles or the rectum. Neoplastic cells can develop the ability to migrate from the place of origin to another part of the body, through the bloodstream and the lymphatic system. These can proliferate and constitute secondary tumors. Prostate cancer most often metastasizes to bones, lymph nodes and can invade the rectum, bladder and ureters, through a local diffusion mechanism.
| Benign tumors | Malignant tumors (prostate cancer) |
|
|
Adenocarcinoma is the most frequent histotype of prostatic neoplasms (it represents about 95% of malignant tumors).
However, there are other cancers, which differ in clinical presentation and course, including:
- Small cell carcinoma (originates from neuroendocrine cells);
- Ductal adenocarcinoma (originates from the cells of the prostatic ducts);
- Mucinous carcinoma (characterized by mucus production);
- Adenosquamous or squamous carcinoma;
- Mesenchymal neoplasms (such as sarcomas or liposarcomas);
- Primary lymphoma of the prostate.
Once the type of cancer has been diagnosed, the doctor will also need to consider:
- The degree of the tumor (how abnormal cancer cells behave);
- The stage of cancer, including if it has spread (metastasis) and where it has spread;
- Prognostic factors (particular characteristics that could influence the course of the disease);
- Survival statistics for the particular type and stage of cancer.
Prostate cancer Video - Causes, Symptoms, Cures
X Problems with video playback? Reload from YouTube Go to Video Page Go to Wellness Destination Watch the video on youtubeCauses
The exact causes of prostate cancer are not yet completely understood, but researchers have identified several predisposing factors and are trying to learn how these can induce neoplastic transformation.
Generally speaking, prostate cancer occurs when abnormal cells within the prostate grow uncontrollably. This event is caused by changes that affect the genetic material of the prostate cells and can induce an alteration of the mechanisms that control the cell cycle, thus favoring the formation of tumor masses. Current scientific research is aimed at understanding genetic alterations (and their combinations), which increase the risk of developing prostate cancer.
Risk factors
Some risk factors are implicated in the development of prostate cancer:
- Old age. Prostate cancer is very rare in men under the age of 40, but the chance of developing the disease increases rapidly after age 50. About 6 out of 10 cases are found in patients over the age of 65.
- Race / Ethnicity. Prostate cancer is more common in some ethnic and racial groups than in others, but the reasons for these differences are not clear. In particular, African American men have a higher risk of developing the disease and a higher probability that this is an aggressive form.
- Family predisposition for prostate or breast cancer . Men who have a blood relative (father or brother) affected by prostate cancer, have a risk of getting sick 2-3 times greater than subjects without familiarity; this risk increases further if there is more than one affected relative in the family and if the disease has been diagnosed before the age of 65 years. Furthermore, the risk appears to be slightly higher for men from families with a history of breast cancer. In particular, the probability of developing prostate cancer is greater in the presence of the mutation of some genes, such as BRCA1 and BRCA2, also involved in the onset of breast and ovarian tumors.
- Lifestyle. Obesity and lack of exercise can promote the development and growth of prostate cancer. The risk is greater for men who consume foods rich in saturated fats, in a diet low in fruit and vegetables. Most studies found no obvious link between smoking and prostate cancer.
- Inflammation of the prostate. Some studies have suggested that prostatitis could be linked to an increased risk of prostate cancer, while other research has not found such evidence. The link between the conditions is not yet clear, but it is the object of further study.
Complications
Prostate cancer can cause complications both in the immediate vicinity and in the rest of the body. Questeincludono:
- Urinary incontinence. Prostate cancer can cause bladder control problems (example: occasional leakage of urine, overactive bladder, etc.). Depending on the severity and cause, these problems can be managed with drugs, catheterization or surgery.
- Erectile dysfunction. Impotence can represent the outcome of the growth of the tumor mass, but also a complication of its treatment through surgery or radiotherapy. The patient may be unable to achieve or maintain a satisfactory erection or engage in sexual activity. Several drugs and medical devices are available to help treat this problem.
- Metastasis. During more advanced stages, cancer cells can spread to adjacent organs or migrate through the bloodstream or lymphatic system, thus forming new tumors in other parts of the body. The most common metastatic sites of prostate cancer are lymph nodes and bones, where they can cause bone pain and pathological fractures. Once prostate cancer has spread to other parts of the body, it can still respond to treatment and can be controlled, but can hardly be cured.
CONTINUE: Prostate Cancer - Diagnosis and Treatment »



