Generality
Cardiac tamponade is a severe form of pericardial effusion, in which there is a large increase in pericardial fluid.

Brief anatomical reference: what is the pericardium?
The pericardium is the membrane that surrounds the heart and the root of the main blood vessels (aorta, pulmonary arteries, hollow veins and pulmonary veins). It consists of two layers, one more external and one more internal.
- The outermost layer is the so-called fibrous pericardium .
- The innermost layer, however, is the serous pericardium ; it adheres perfectly to the heart and to all its inlets and consists of two sheets of cellular tissue, called parietal leaflet and visceral leaflet. These two sheets do not adhere to each other, but are separated by a cavity, called the pericardial cavity, inside which the pericardial fluid is contained.
The pericardial fluid, whose normal volume is about 20-50 ml, serves to reduce friction and rubbing between the layers that make up the pericardium.
DANGER FUNCTIONS
In addition to acting as a lubricant, the pericardium has several other functions.
It is essential to fix and maintain the heart in the correct position within the mediastinum .
It acts as a defensive barrier against viral or bacterial infections that could compromise cardiac activity.
Finally, avoid excessive dilation of the heart when it is affected by particular pathologies.
What is cardiac tamponade
We speak of cardiac tamponade when the pericardial fluid, contained in the pericardial cavity, increases in volume and compresses the heart, hindering the latter in its action of pumping blood. This is an emergency that seriously endangers the affected patient.
Based on the causes of cardiac tamponade, the pericardial fluid can be enriched with blood, pus, blood clots or gaseous substances. The presence of these elements also contributes to increasing the friction between the layers of the pericardium, thus making the patient feel a painful chest sensation.
THE DANGEROUS PAYMENT

Figure: comparison between a normal heart (left) and a heart with pericardial effusion (right). The arrows indicate the pressure that the accumulated fluid exerts on the heart. From the site: cardiachealth.org
The increase of fluid in the pericardial cavity is a clinical situation known as pericardial effusion . The latter can be more or less serious, depending on the amount of liquid accumulated. If the volume is considerable, there are more dramatic symptoms and complications for the patient: one of these is cardiac tamponade.
It cannot be ruled out that a slight pericardial effusion will worsen and become severe: in these cases, we notice the change because the affected individual shows clear signals.
Epidemiology
Cardiac tamponade is a rare pathological condition: in the United States, it has been calculated that about 2 out of 10, 000 people suffer from this disorder each year.
In young adults, its appearance is mainly due to thoracic trauma or the AIDS virus. In elderly people, on the other hand, cardiac tamponade is the result of chronic renal dysfunction, sometimes even dramatic.
Causes
The condition of cardiac tamponade arises when there is an important accumulation of pericardial fluid between the sheets of serous pericardium.
But what are the causes that trigger a cardiac tamponade?
Very often, this disorder is due to a pericarditis, but this is not always the case. It can, in fact, arise after a chest injury, after a heart surgery, due to the presence of a lung tumor, an aortic dissection, an aortic aneurysm, etc.
PERICARDITIS
The term pericarditis refers to the inflammation of the pericardium. It can arise for many reasons, sometimes unrecognizable even after a careful diagnosis.
The pericarditis that most frequently causes cardiac tamponade are those due to:
- Lung cancer and chest cancer
- Heart attack ( heart attack )
- Viral infections (especially the AIDS virus ) and bacterial ( tuberculosis )
- Autoimmune diseases (in particular lupus, rheumatoid arthritis, dermatomyositis and scleroderma)
- Chronic kidney diseases
- Post-surgical heart complications
- Radiotherapy (if the patient underwent this treatment for the treatment of a tumor)
NB: an autoimmune disease arises when an organism's immune system turns against the organism itself, attacking its tissues.
OTHER CAUSES
Other causes of cardiac tamponade are:
- Heart thoracic traumas, mainly due to road accidents
- Surgery for the heart or chest (insertion of a pacemaker, chest drainage, etc.) or diagnostic examinations for the heart (angiography and cardiac catheterization)
- Rupture of an aortic aneurysm
- Aortic dissection
- Taking certain medications: for example, minoxidil, isoniazid or hydralazine
- Hypothyroidism
- Tumors of the thoracic organs or tumor metastases
Some pathological conditions in this list are the same ones that cause pericarditis. However, this is not a repetition, but only the fact that, in some cases, there is a cardiac tamponade without necessarily having developed a pericarditis.
Symptoms and Complications
When cardiac tamponade occurs, the heart is compressed and can no longer perform its normal functions. The liquid, in fact, compresses the cardiac cavities (the ventricles in particular), preventing them from expanding completely and filling themselves with blood adequately. It follows that, when the heart contracts due to blood circulation, it is insufficient and ineffective. In other words, the heart, compressed as it is by the accumulation of pericardial fluid, is not able to make the blood flow in all the districts of the body.
What effects can this condition have?
SYMPTOMS OF CARDIAC PADDING
The typical symptoms of cardiac tamponade, accused by the patient, are: anxiety, agitation, sense of general weakness, chest pain (sometimes spread to the shoulder and neck), dyspnoea (difficulty breathing), palpitations, tachycardia, sense of fainting, vertigo and loss of consciousness.
Moreover, some postures intensify the painful sensation suffered by the patient: for example, sitting or leaning forward with the torso.
SIGNS
The signs of cardiac tamponade, detectable by the doctor, are different. Probably, among these, the most characteristic is arterial hypotension (low pressure at the level of the arteries), which is established after the heart is no longer able to pump blood circulating adequately.
Hypotension can sometimes be associated with distension of the jugular veins (due to poor return of blood to the heart) and muffled heart tones. The simultaneous presence of these three signs is called the Beck triad .
Another equally typical sign, perceived by the doctor using a stethoscope, is the sound of something rubbing. This noise is the result of greater friction between the layers of pericardium and the abnormal pericardial fluid, filled with inflammatory cells, blood clots, etc.
Other signs can be:
- Paradoxical pulse (strong decrease in systolic pressure during inspiration)
- Tachypnea (increased respiratory rate)
- Hepatomegaly ( enlarged liver )
- Cyanosis
- Pulmonary edema
COMPLICATIONS

Figure: the distension of the jugular veins (or turgor of the jugular veins) is a possible sign of cardiac tamponade. This phenomenon is due to the difficulties encountered by the blood returning to the heart (insufficient venous return). From the site: //it.wikipedia.org/
An individual with cardiac tamponade can suffer severe organ damage and enter a state of shock due to the severe absence of oxygen.
If the patient does not receive relief and appropriate care, he can easily die.
Diagnosis
The clue that can lead the doctor to suspect an ongoing cardiac tamponade is the detection of the Beck triad (hypotension, distension of the jugular veins and muffled heart sounds). However, since these three signs are not always present simultaneously in all patients, other tests and tests must be used.
Therefore, for a correct diagnosis of cardiac tamponade, one must resort to:
- Echocardiogram
Through an ultrasound of the heart, one can see the pericardium dilated by the liquid and the cardiac cavities (in particular the ventricles) compressed.
- Chest x-ray
Shows the enlarged heart, following the accumulation of pericardial fluid.
- Computerized axial tomography ( TAC )
Provides detailed images of the heart and pericardium. It is also essential to clarify the causes and to exclude pathological situations with similar symptoms. Low doses of ionizing radiation are used, slightly harmful to the patient.
- Nuclear magnetic resonance
Show the pericardium and its possible anatomical changes.
- Coronary angiography
It is useful for the doctor to see what the blood flow inside the blood vessels that supply the heart is.
- Electrocardiogram ( ECG )
Cardiac tamponade determines a particular heartbeat, recognizable by ECG.
OTHER DIAGNOSTIC TESTS
Alongside these diagnostic tests (which the doctor needs to confirm or rule out the presence of a cardiac tamponade), various checks are performed on the patient's blood and urine to determine what causes the disorder.
| Origin of the sample to be analyzed | Measured parameter |
Blood |
|
Urine |
|
Treatment
To effectively treat cardiac tamponade one must:
- Intervene on symptoms
- Take action on the causes
Therapeutic treatment of symptoms alone has temporary effects and is not enough; it is necessary to go to the origin of the disorder, to be able to solve it definitively. Without this double intervention, the tamponade therapy would fail and the risk of a relapse would be more than concrete.
HOSPITALIZATION IS REQUIRED?
Cardiac tamponade is an emergency, therefore it requires hospitalization for the good of the patient and to ensure the most appropriate care.
THE IMMEDIATE TREATMENT OF SYMPTOMS
The patient suffering from cardiac tamponade needs immediate relief .
The first operation to do is to supply oxygen, to avoid the possible onset of a state of shock. Subsequently, pressure must be restored to physiological levels. To do this, positive inotropic drugs ( dobutamine ) are used, which improve myocardial contractility, and measures to favor venous return to the heart, such as the raised-leg position.
THE SURGICAL TREATMENT OF SYMPTOMS
Once the patient has stabilized and is under observation, surgery can be performed. The most used method is pericardiocentesis ; however, if this should not be sufficient, other, unfortunately more invasive, procedures also help.
- Pericardiocentesis : it is the drainage, through aspiration, of the excess pericardial fluid. To aspirate the fluid, a sterile, needle-like catheter is used, which is led to the pericardium. The incision point is under the xiphoid process of the sternum (subxiphoid incision).
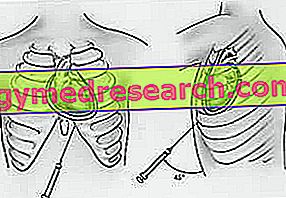
- Thoracotomy and peritoneal shunt (or in the pleural cavity) : the thoracotomy is the opening of the chest and allows the surgeon to have access to the internal organs. After this first operation, the shunt (or discharge) of the excess liquid from the pericardium towards the peritoneal or pleural cavity is performed by means of a catheter. The shunt involves the removal of a small portion of pericardium. Usually, this procedure is used when there are blood and blood clots in the pericardial fluid.
- Pericardiectomy : It is the removal of the pericardium. It is used in the most serious cases and only if strictly necessary. Usually, it is practiced for those for whom a repeat offense is predictable. This is a very delicate operation, which in one case out of 20 can determine the death of the patient.
THE TREATMENT OF CAUSES
The cure of the causes of cardiac tamponade is fundamental to avoid relapses and to save the patient's life. Clearly, care varies from patient to patient and only a correct diagnosis guarantees the most appropriate therapeutic choices.
Prognosis
The prognosis for a patient with cardiac tamponade depends on three factors:
- Speed of diagnosis
- Promptness and accuracy of intervention
- Causes of cardiac tamponade
Early diagnosis of a cardiac tamponade is essential to avoid unpleasant consequences (heart attack or shock), sometimes even lethal.
It is also essential, then, to intervene promptly and with the most appropriate care: only in this way can the patient be guaranteed a good recovery and a return to a normal life.
Finally, the causes also play a critical role, because, for some of them, the therapy is more complicated and not as effective compared to other less serious situations of cardiac tamponade.