Generality
The mini-pill is an oral contraceptive based on a progestin hormone .
This drug works by thickening the mucus of the uterine cervix and altering the lining of the uterus (endometrium). As a result, the spermatozoa struggle to ascend along the female genital apparatus and the implantation of the possibly fertilized egg is disadvantaged.

To get the maximum effectiveness, it is necessary to take the mini-pill every day, always at the same time and without interruption.
What's this
The mini-pill is a contraceptive composed exclusively of progesterone. Unlike other birth control pills, this oral drug does not contain estrogen .
In the minipill, the synthesis progesterone used for its formulation can be norethisterone, levonorgestrel or ethinodiol.
Note
The dose of progestin hormone contained in a minipillole is lower than the quantity of the same in the combined contraceptive pill ( or estroprogestinica ) .
What is it for?
The mini-pill is an oral drug that can be taken by women who wish to prevent conception.
This contraceptive acts mainly by the continuous action of small doses of progesterone, which:
- They thicken the mucus at the level of the uterine cervix, making it less suitable for the passage of spermatozoa that want to reach the egg cell;
- They alter the endometrium, in such a way as to disadvantage the implantation of the fertilized egg at the level of the uterus.
Like other birth control pills, then, the minipillola blocks ovulation: progesterone inhibits the secretion of LH (luteinizing hormone), thus preventing the release of the mature egg cell into the fallopian tubes. In this case, the degree of efficacy is variable and depends on the quantity of synthetic progesterone present in the product: at low progestin doses it corresponds to a percentage of inhibition of ovulation equal to 50%, while to the intermediate ones it is higher than 97%.
The mini-pill is a reversible contraceptive solution; the interruption of his assumption therefore leads to the immediate restoration of conception skills.
When it is prescribed
The doctor can prescribe the mini-pill in the following cases:
- Estrogen intolerance . Some women choose the mini-pill because they cannot or do not want to take contraceptives containing estrogens, due to possible drug interactions or associated side effects.
- Coagulation dysfunctions . In the presence of an abnormal formation of blood clots in the legs, in the myocardium or in the lungs, or if the patient has a greater risk of incurring thromboembolism, the doctor may recommend taking the mini-pill.
- During breastfeeding . For many years, the estrogenic component of the combined contraceptive pill was thought to inhibit the production of breast milk (lactation). Although recent research has shown that these drugs do not affect breastfeeding, many doctors and patients place greater trust in the use of the mini-pill during the breastfeeding period.
The doctor may also indicate the minipill in the treatment of some forms of dermatitis that appear to be related to the menstrual cycle.
How to use?
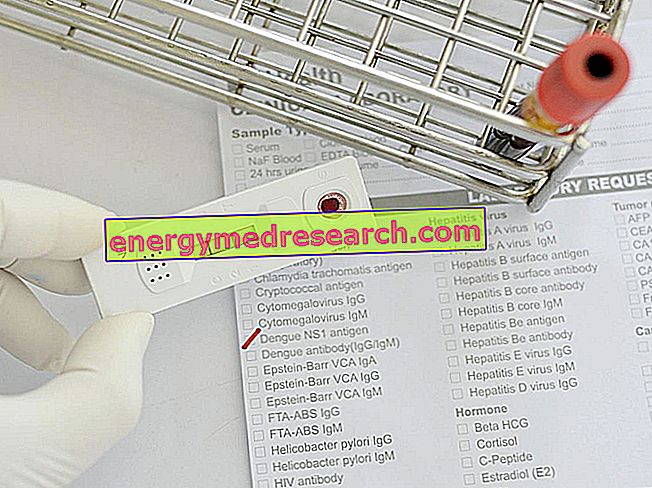
As for the combined pill, even in the case of using the mini-pill, before starting to take it, consult a doctor and / or a gynecologist to carry out the following checks:
- General visit;
- Gynecological and breast examination;
- Blood pressure control;
- PAP test;
- Complete urine test;
- Blood test: blood glucose, cholesterol (HDL), triglycerides, transaminases, etc.
These checks must be repeated every year.
For correct use, taking the mini-pill should start on the first day of the menstrual cycle (which corresponds to the first day of menstruation). From this moment on, the patient must use the drug every day, always at the same time, until she decides to stop the contraceptive therapy.
The mini-pills must be taken without pauses, so once a package is finished, the woman must immediately start another one (in other words, the use is continuous).
Currently, there are two subtypes of minipill:
- 3-hour mini-pill (eg Micronor and Norgeston);
- 12 hour mini-pill (eg Cerazette).
The difference between these drugs is the period of time within which the intake is still effective in preventing conception. This means, for example, that the minipillule contraceptive protection is valid only if it is taken before 12 hours have elapsed from the usual time of use established.
If taken correctly, the mini-pill has a contraceptive efficacy that reaches 97%. Any forgetfulness in the assumption could render it ineffective, especially if it is delayed beyond the time interval for the given product in use.
If the delay is excessive it is advisable:
- Continue with the minipill at the established daily usage time;
- In the two days following the forgetfulness, use an additional contraceptive, in the case of possible sexual relations.
Advantages and disadvantages
Thanks to the low concentration of progesterone in its formulation and the absence of estrogens, the minipillola has - compared to the combined contraceptive pill - some advantages :
- It is recommended for women who cannot take estrogen or suffer from the side effects produced by the hormones themselves.
- It interferes only marginally with coagulation, lipid metabolism and arterial pressure;
- Many side effects of the combined pill (water retention, breast tension or tenderness, etc.) tend not to be present, precisely because the hormonal load is very low;
- Does not alter vaginal pH;
- It can be taken immediately after birth, as it does not interfere with lactation;
- It can be prescribed to women of any age;
- It allows a rapid recovery of fertility, after its interruption.
However, compared to the combined contraceptive pill, the minipill also has disadvantages :
- Need for precise recruitment, without the possibility of errors: for an optimal contraceptive coverage, the minipill should be taken every day, always at the same time, otherwise it is no longer safe;
- Tends to cause irregularities in the menstrual cycle or amenorrhea (disappearance of menstruation).
- Efficacy can be compromised by the concomitant intake of some drugs (antiepileptics, antibiotics and antivirals) or natural substances (eg hypericum and charcoal);
- The failure rate of this contraceptive method is considered to be higher than that of other hormonal contraceptive methods. The coverage from unwanted pregnancies is lower than the combined pill.
Furthermore, it should be remembered that the mini-pill is a contraceptive method that:
- It does not protect against sexually transmitted diseases (STDs);
- Requires medical prescription.
Side effects and contraindications
The mini-pill is a safe and well-tolerated contraceptive method. Undesirable effects resulting from its intake are rare and of modest magnitude.
These include:
- Fatigue;
- Mastalgia associated with increased breast size;
- Acne;
- Increased body weight;
- Headache;
- Nausea and vomit;
- Mood swings;
- Changes in libido;
- Irregularity of the menstrual cycle, absent or light periods and intermenstrual blood loss (spotting);
- Abdominal cramps;
- Depression.
These disorders usually manifest themselves in the first few months of use of the mini-pill, and then gradually diminish, until complete disappearance.
In the long term, the use of the minipill may predispose to the development of ovarian cysts. These formations are not dangerous and tend to resolve spontaneously; however, in some women, they can cause annoying pelvic pain.
If the contraceptive method fails and conception takes place, the probability that the pregnancy is ectopic is slightly higher.
The use of the mini-pill is contraindicated in the following cases:
- Concomitant use of certain drugs that reduce the effect of minipill, such as, for example, rifampicin and rifabutin (antibiotics), carbamazepine, oxcarbazepine, phenytoin and phenobarbital (antiepileptics), hypericum and antiretroviral medicines used to treat HIV infection and AIDS.
- Presence of a cardiovascular and / or hepatic disease;
- Bariatric surgery;
- Atypical uterine bleeding;
- History of breast cancer (ongoing or previous) or family predisposition for this neoplastic disease;
- Predisposition to the development of ovarian cysts;
- Difficulty taking the pill daily at the same time, due to changes in work shifts or other factors.
The contraceptive efficacy of the mini-pill could be compromised after episodes of vomiting or severe diarrhea (within 5 hours after administration).
Tips
- Consult your doctor to establish a start date for taking the mini-pill. For those who did not use hormonal contraceptives in the previous month, the first tablet should be taken from the first day of the menstrual cycle (which coincides with the onset of menstruation).
- To obtain maximum protection against a possible conception, use an additional contraceptive measure (generally, a "barrier" method, such as a condom is recommended) for at least seven days after the start of minipillary therapy.
- The mini-pill should be taken every day for 28 days; subsequent assumptions must always be made at the time of daily use established with the first administration. Do not take breaks between the minipill packs: before finishing the one in use, get or keep the next box ready. Unlike combined contraceptive pills, mini-pill blisters do not contain a week of inactive medication.
- In case of appeal the previous month to other contraceptive methods, it is important to start taking the mini-pill:
- The same day of removal of the vaginal ring or transdermal patch;
- The day after taking the last combined active pill.
When there is an interval free from hormonal contraceptives (ie the minipillule is taken the day after the ring or patch is removed or after the combined inactive pill), an additional contraceptive method must be used for the first week of therapy.
- If you do not remember to take the mini-pill and have unprotected sex, consult your doctor about an emergency contraception method.
- In case of important or unusual side effects, consult your doctor.
Alarm signals
In the presence of these symptoms, contact your doctor immediately:
- Strong bleeding that lasts a long time or is unusually painful;
- First appearance or worsening of migraine-type headache, or more frequent appearance of an unusually strong headache;
- Sudden visual, hearing or speech disorders;
- First signs of thromboembolic events (eg unusual swelling of the legs or stinging pains during breathing);
- Significant increase in blood pressure (in repeated measurements);
- Appearance of jaundice and generalized itching;
- Abdominal pains;
- Sudden onset of dizziness, fainting, feeling of weakness and sensitivity disturbance;
- Pregnancy (or suspected conception).
These manifestations can be the consequence of serious health problems, which are not necessarily the consequence of hormonal contraception, but require immediate suspension.
- In agreement with your doctor, it is recommended to discontinue use of most progestogen contraceptives, at least four weeks before a planned surgery and during prolonged immobilization (eg after an accident or an operation).
Given that reliable contraception may still be necessary, it is advised to identify a suitable contraceptive method with your doctor.
To remember
- The patient can start using the mini-pill at any time of the day. As part of their daily habits, doctors advise you to choose a comfortable time, so as to reduce the risk of forgetting to take them.
- After the first administration, the woman must take the mini-pill every day, always at the same time, without pauses, until she decides to stop the therapy (so that the interval between the two tablets is always 24 hours) . The hiring time must not change, even if a minipillola is forgotten.