Generality
Esophageal diverticula are congenital or acquired saccular extroflections of the esophagus wall, communicating with the lumen of the esophagus. In relation to the formation mechanism, we distinguish between diverticula from drive and from traction. The former are due to the gradual flexion of the mucosa and submucosa through an area of weakness of the muscular wall, due to an increase in intraluminal pressure. The latter, on the other hand, occur as a result of tensile forces exerted on the esophageal wall, due to an adjacent inflammatory process (example: involvement in inflammation of mediastinal lymph nodes in tuberculosis). Esophageal diverticula are often asymptomatic, but are sometimes associated with dysphagia and symptoms of variable severity that can be related to esophageal dyskinesias.
Diagnosis
The results of the physical examination are often normal, as the patients are frequently asymptomatic. However, many patients report episodes of dysphagia, chest pain or food regurgitation.
Radiographic investigations of the esophagus or upper gastrointestinal tract allow the detection of many non-symptomatic diverticula.
- Chest radiography and computerized tomography allow the identification of large esophageal diverticula, which can appear as structures filled with air and / or liquid in communication with the esophagus.
- The fluoroscopy of the esophagus (barium radiography) is generally the diagnostic technique of choice: a sequence of radiographic images is performed, after the ingestion by the patient of the so-called "binary meal", a contrast medium containing barium sulfate, which appears clear to the development of the radiographic plate (as the radioisotope is opaque to X-rays).
- The technique can be achieved by " double contrast " (binary meal + air produced by the simultaneous ingestion of sodium bicarbonate, which reacts with gastric acids and rises through the esophagus), to allow a better distension of the bowel and highlight any macroscopic mucosal irregularities. Barium radiography is useful for the diagnosis of intramural esophageal pseudodiverticula, while the "bariate meal" provides more diagnostic information in symptomatic patients, with mid-thoracic or epiphrenic diverticula. The technique is excellent for defining the structural aspect of esophageal diverticula and provides clues related to motility disorders determined by the presence of these formations.
- The gastro-esophageal manometry allows to measure the time and strength of the contractions and relaxations of the muscular valves at the level of the upper esophageal sphincter (SES) and lower (SEI). More precisely, the test allows to highlight the association with the alterations of motility or with the presence of a muscular hypertonus, which determines an increased resistance to movements:
- at the level of the upper esophageal sphincter, for Zenker's diverticulum;
- at the level of the lower esophageal sphincter, for epiphrenic diverticula.
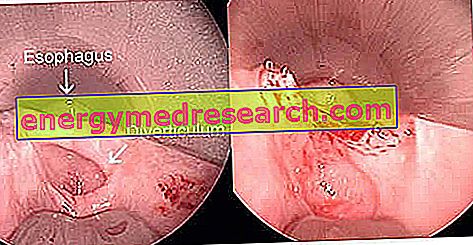
- In the case of obvious symptoms such as the manifestation of dysphagia and odynophagia (painful sensation during swallowing), an esophageal gastrousodenoscopy (EGDS) is indicated, an endoscopic examination of the upper digestive tract, which allows the exclusion of structural pathological conditions associated with the diverticula of the esophagus, such as strictures or neoplasms.
Treatment
In general, asymptomatic or minimally symptomatic diverticula do not require treatment.
In many patients with esophageal diverticula, dysphagia is related to the alteration of basic motility, so therapy must be directed to treat this disorder. For example, the treatment of intramural esophageal diverticulum is directed at the underlying stenosis or dysmotility.
Only in certain cases, in which the esophageal diverticulum reaches considerable dimensions, or if it is associated with a disabling symptomatology, it is possible to evaluate the possibility of resorting to surgical excision (resection). The indications for the surgical treatment of esophageal diverticula are well represented by three characters: symptomatic, voluminous, invalidating .
Therapeutic options may also include:
- Botulinum toxin injection at the level of the lower esophageal sphincter (with transient effect, from 1 to 3 months).
- Heller's esophageal myotomy (surgical resection of the bundles of smooth muscle tissue surrounding the esophagus).
Some surgical approaches are shown below:
| Esophageal diverticula | Type of intervention indicated | Procedure |
| Zenker's diverticula | Video-assisted esophagus-diverticulostomy via trans-oral route | It foresees an intervention under general anesthesia and the introduction of a special endoscopic instrumentation (diverticuloscope + linear saturator) which allows the creation of a common cavity between the diverticulum and the esophagus, to correct the condition. |
 | ||
Zenker's diverticulum before and after the esophagus-diverticulostomy - Source: //stanfordhospital.org/ | ||
| Epiphrenic diverticula | Diverticulectomy + myotomy and anti-reflux plastic | Technique performed by laparoscopy which can be associated with an esophageal myotomy of Heller (extramucosal esophageal incision) and an anti-reflux plastic. |
| Parabronchial diverticula | Thoracotomy diverticulectomy | Invasive surgical method which involves opening the chest to perform the diverticulum resection. |
Surgery resolves the stenosis definitively, with clinical and radiological remission of the disease. In recent years, non-invasive techniques have been perfected that guarantee good results and modest post-operative pain.
Diet and Lifestyle
- Do not lie down (or bend) immediately after main meals
- Sleep with two pillows, to facilitate emptying of the esophagus and limit stagnation of food
- Avoid large meals
- Avoid taking coffee, mint, chocolate, fatty foods and alcohol
- Reduce acidic foods that can irritate the walls of the esophagus: juices, citrus juices, tomatoes and pepper.