What is Prostatic Biopsy?
Prostate biopsy is a diagnostic test aimed at the collection of small prostate tissue samples, subsequently observed with an optical microscope to confirm or exclude the presence of prostate cancer.
How to do it? Possible complications. Preparation
Indications
When is it necessary?
The finding of one or more of the following elements is a common indication for prostatic biopsy:
- high blood levels of PSA (prostate specific antigen);
- suspicious pictures emerged during transrectal prostatic ultrasound;
- perception of abnormal formations during rectal exploration of the prostate (the doctor introduces his or her index finger into the patient's anus and feels the gland through the intestinal wall).
Prostate biopsy is therefore necessary whenever there is a well-founded suspicion of prostate cancer, a disease that represents - even if only in certain respects - the most common type of cancer among men. Fortunately, many prostate tumors are benign or slowly evolve, remaining circumscribed for a long time in the gland without creating significant disorders (the incidence of these tumors is very high, while mortality is extremely low, which is why they say "they die more men with prostate cancer than prostate cancer "). Unfortunately there are also not too frequent cases in which the disease develops rapidly and forms metastases already at an early stage (the incidence of these malignant tumors is relatively low, but the mortality is quite high).
Prostate cancer is very rare before the age of forty-five and even if in this regard there are no precise screening schemes, starting from this age it is important to undergo regular checks of the gland, especially in the presence of risk factors - such as the familiarity with the disease - or suspect symptoms, such as difficulty urinating, pain and burning sensation when urinating, haematuria and a sense of incomplete emptying of the bladder (bladder tenesmus). Since the usefulness of these "screening" tests in asymptomatic people is debated, it is important to consult your doctor to evaluate whether or not to undergo tests such as PSA dosing and digital rectal exploration.
How do you do it?
Unfortunately, non-invasive tests like TAC, Nuclear Magnetic Resonance and PET cannot accurately identify this type of tumor, which is generally very small, which is why it is necessary to take a sample of prostate tissue to be subjected to histological examinations.
Transrectal biopsy
During prostate biopsy, the patient is generally lying on his side, with the thighs flexed towards the chest or, alternatively, in the "gynecological" position (supine with legs apart).
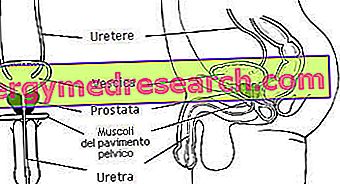
Once assumed the body attitude suggested by the doctor, the urologist performs a preventive digital exploration of the rectum and prostate. Thus ascertained the absence of contraindications, a well lubricated ultrasound probe is inserted into the anus, which allows the prostate to be visualized on the appropriate screen going up the rectum. In this regard the instrument uses a beam of sound waves, evaluating the consequent degree of reflection of the tissues; there is therefore no danger associated with ionizing radiation.
Through the way opened by the probe, with the help of ultrasound images, the doctor injects a small dose of anesthetic (lidocaine) near the prostate, then letting the drug act for a few minutes. Taking advantage of a special biopsy needle and ultrasound images, the doctor takes on average 8/16 fragments of prostate, depending on the size of the same, the results of previous biopsies and the possible clinical suspicion given by rectal exploration. Meanwhile, the ultrasound probe allows the urologist to continuously monitor the prostatic areas reached by the needle.

The technique just described is called transrectal prostatic biopsy; a variant of this method, even if used less frequently, involves access to the prostate through the perineum.
Both methods have proven to be effective and safe, which is why the choice between the two depends essentially on the preferences of the operator. Trans-perineal and trans-rectal techniques under digital control, therefore without the aid of ultrasound, have instead fallen into disuse. The biopsy of the transurethral prostate is also quite rare with the aid of a cytoscope.