Causes and generalities
The term dehydration indicates an excessive depletion of body water, which under normal conditions constitutes about 80% by weight of the child. The possible causes of origin are quite numerous, often accumunate from the fever rise, from the vomit, from the diarrhea and / or from the temporary impossibility of drinking.

Other causes of dehydration include bacterial gastroenteritis ( Salmonella, Escherichia coli, Campylobacter, Clostridium difficile ), type I diabetes, cystic fibrosis and malabsorption syndromes.
Symptoms
The physical examination is very important to recognize the degree of dehydration of the child, which compared to the adult is more exposed to major water losses. The ideal would be to calculate this deficit by comparing the child's usual weight with that measured at the suspicion of dehydration.
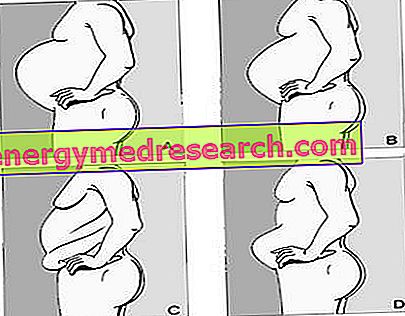
In mild forms, dehydration is 3% -5% (difference between the two weights) and the baby has essentially a normal picture.
In moderate dehydration, water loss is 6-9%; the patient becomes suffering, irritated (cries more even if the tears are scarce), with tachycardia, cold skin, dry lips and mucous membranes, haloed eyes, dry and anelastic skin, sunken fontanelle (in the infant), reduction of tears and of urinary output.
These symptoms deserve to be readily brought to the attention of the pediatrician.
The severe form develops with a dehydration of more than 10%; the aforementioned symptoms are associated with lethargy (slowed-down activities, sleep, difficulty waking up), marked tachycardia and tachypnea, lengthening of the capillary filling *, poor turgidity of the skin and poor emission of urine (dryness of the diaper).
These symptoms deserve prompt access to the emergency room, where, after carrying out a few but necessary laboratory tests, an assessment will be made of the condition of the salt and water balance of the small (which will be monitored over time) and a correct and adequate correction of water losses and of salts by means of parenteral infusions.
* By applying pressure to the patient's palm or fingertip, blood is "squeezed" out of the underlying tissues. Releasing the pressure, the skin appears lighter, but the blood returns to perfuse the tissues, restoring the original color. The capillary filling time is precisely the time in which the normal skin color returns: if greater than 2 seconds, the test is defined as positive.
What to do?
Estimated the severity of dehydration, the next step is to calculate how many fluids to administer to the patient. This operation can be easily carried out remembering that a liter of fluids weighs a kilo; therefore, a child of 20 kilos with a dehydration of 5% has lost a kilo of body weight (0.05 x 20 kg = 1 kg); therefore, it has a fluid deficit of one liter.
In mild and moderate dehydration oral hydration therapy is the first choice method; it is based on the administration of special hyposmolar drinks, which can be purchased in pharmacies, such as Pedialyte or Infalytr.
For children over the age of two, rehydration drinks for athletes can also be used. The guidelines recommend starting therapy by administering 5 ml of rehydration solution every five minutes, gradually increasing it according to tolerability. More generally, therefore, it is important to administer small amounts of liquids at very frequent intervals. For no reason use carbonated drinks and fruit juices, which - being solutions rich in sugar, therefore hyperosmolar - would worsen diarrhea and dehydration. Simple water, on the other hand, normally does not contain enough mineral salts and can cause electrolyte imbalances, with the risk of convulsions.
If you don't have rehydrating drinks available, the ideal is to prepare them independently, dissolving four teaspoons of sugar, half a teaspoon of salt, half a teaspoon of potassium chloride and half a teaspoon of baking soda in one liter of water.
Normal feeding will be resumed as soon as the baby is able to tolerate it.
At the hospital level, when the child presents with severe dehydration, or if it is not possible to rehydrate orally due to persistent vomiting, intravenous therapy is used (infused with 20 ml boluses / kg until the shock is resolved ). Vomiting, by itself, is not a contraindication to oral rehydration and can be resolved through the use of antiemetics (obviously as recommended by the pediatrician).