Definition
Also known as Hughes' syndrome or APS, the anti-phospholipid antibody syndrome is a complex autoimmune disease, characterized by recurrent abortions, thrombocytopenia, venous or arterial thrombosis, and the presence of specific auto-antibodies, called antiphospholipids.
Causes
We speak of a syndrome of primary anti-phospholipid antibodies when it does not depend on autoimmune diseases; the secondary form, on the other hand, is of an autoimmune nature and is closely related to lupus erythematosus. Predisposing factors include: abuse of some drugs (hydralazine, phenytoin, Amoxicillin), infections (hepatitis C, HIV, malaria), genetic predisposition, development of antiphospholipid antibodies.
Symptoms
The anti-phospholipid antibody syndrome is characterized by the appearance of thrombotic manifestations affecting arteries, veins or capillaries of any anatomical district; the syndrome can degenerate into pulmonary embolisms, ischemic cerebral stroke, myocardial infarction, occlusion of visceral arteries or deep vein thrombosis. The anti-phospholipid antibody syndrome becomes very problematic when it occurs in pregnancy, since it can cause fetal growth retardation, premature birth, preeclampsia and placental insufficiency.
Information on drugs for anti-phospholipid antibody syndrome is not intended to replace the direct relationship between health professional and patient. Always consult your doctor and / or specialist before taking Drugs for Anti-phospholipid Antibody Syndrome.
drugs
Patients who experience high levels of antiphospholipid antibodies in the blood must undergo specific analysis, since the presence of these abnormal antibodies could trigger very serious consequences, such as thrombosis in general.
The drugs of choice for the treatment of the anti-phospholipid antibodies syndrome are definitely the anticoagulants, to be used periodically, and the antiplatelet agents. Only in cases of extreme gravity (catastrophic syndrome caused by antiphospholipid antibodies), it is possible to use immunosuppressive drugs, immunoglobulins and, possibly, resort to plasmapheresis.
During pregnancy, as mentioned above, the anti-phospholipid antibody syndrome could trigger serious complications, especially for the unborn child; therefore, drug therapy, although extremely complex during gestation, proves necessary, and is essentially based on the administration of anticoagulants, such as heparins and acetylsalicylic acid. Warfarin is not recommended during pregnancy, as it can cause serious side effects, such as birth defects. Only in extreme cases, when the benefits outweigh the risks, it is possible to prescribe the drug to the expectant mother.
Anticoagulant therapy requires constant monitoring of the blood tests of the patient suffering from the anti-phospholipid antibody syndrome.
- Heparin (eg. Heparin Cal Acv, Heparin Sod.Ath, Ateroclar, Trombolisin): heparin is administered in small doses by slow infusion; generally it is combined with another anticoagulant (eg. Warfarin). In general, for the treatment and prevention of thrombotic events in the context of the anti-phospholipid antibody syndrome, it is recommended to take an active dose of 100 units / ml, every 6-8 hours for PVC catheters; alternatively, for the prevention of deep vein thrombosis, take 5000 units of the drug, subcutaneously, every 8-12 hours. Consult your doctor.
Some types of heparin (for example, dalteparin and enoxaparin) can also be taken during pregnancy, in order to avoid the degeneration of the anti-phospholipid antibody syndrome in serious complications. Heparin can also be used in pregnancy to increase the chances of therapeutic success in the context of anti-phospholipid antibody syndrome: approximately, it is recommended to take 5000 units of the drug subcutaneously every 12 hours. The dosage can be changed by the doctor, depending on the severity of the syndrome.
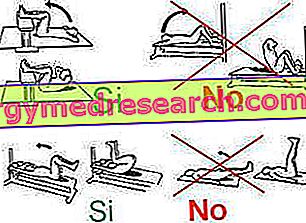
- Enoxaparin (eg. Clexane): for the prophylaxis of venous thrombosis in the context of the anti-phospholipid antibody syndrome, it is recommended to take an active dose of 40 mg, subcutaneously, once a day. The duration of therapy varies from 6 to 14 days. If the patient is obese, it is recommended to follow a low-calorie, healthy and balanced diet, and to practice constant physical activity. The drug can also be taken during pregnancy.
- Dalteparin (eg Fragmin): a low molecular weight drug, to be injected under the skin. The active principle is indicated, in particular, for the prevention of deep vein thrombosis also in the context of the anti-phospholipid antibody syndrome. The drug should be taken by subcutaneous injection at the dose established by the doctor, based on the severity of the condition. The drug may also be associated with acetylsalicylic acid.
- Sulodexide (eg Provenal): the drug (heparin-like) is used in therapy for the treatment of vascular diseases with a high thrombotic risk; in this regard, its administration is sometimes also recommended for the anti-phospholipid antibody syndrome. As an indication, take 2 capsules of 250 ULS a day, before meals.
- Warfarin (eg. Coumadin): for the treatment of anti-phospholipid antibody syndrome, warfarin monotherapy follows a period of treatment with a platelet anti-aggregator. In all likelihood, treatment with this drug will last for life. Even if the dose should be accurately established by the doctor, indicatively, for the prophylaxis of thrombosis (closely associated with the anti-phospholipid antibody syndrome) it is recommended to take 2-5 mg of active, orally or intravenously, once a day or every another day.
- Acetylsalicylic acid (eg Aspirinetta, Cardioaspirin): aspirin can complete a pharmacological program with other antiplatelet agents. In general, aspirin is prescribed at a dosage of 75-100 mg (to be taken per os).
The drug (acetylsalicylic acid) reduces platelet aggregation by lowering the coagulative capacity of the blood; the effect is particularly important for preventing thrombotic events often associated with the anti-phospholipid antibody syndrome.