Generality
Intercostal neuralgia is a rare pathological condition, resulting from damage or malfunction of the intercostal nerves; this condition causes a characteristic pain in the intercostal area.

Additional symptoms may be added to intercostal pain, such as: tingling, numbness, back pain, widespread pain in the chest, left arm and shoulder, etc.
Accurate diagnosis of the causes that trigger intercostal neuralgia is essential for the most appropriate treatment planning.
The latter generally consists of a causal therapy, combined with symptomatic therapy.
Anatomical recall on rib cage and ribs
The thoracic cage is the skeletal structure placed in the upper part of the human body, exactly between the neck and the diaphragm, which serves to protect vital organs (such as the heart and lungs) and important blood vessels (aorta, veins, cavities, etc.).
According to the anatomy manuals, it includes:
- Later, the 12 thoracic vertebrae ;
- Latero-anteriorly, 12 pairs of ribs (or ribs );
- Anteriorly, the costal cartilages and a bone called the sternum .
Each pair of ribs is connected to one of the 12 thoracic vertebrae; obviously, the left ribs emerge from the left side of the aforementioned vertebrae, while those on the right from the corresponding right side.
At their front end, the ribs articulate with the costal cartilages.

The space between the overlapping ribs is called the intercostal space .
In the intercostal space reside the so-called intercostal muscles - which play a fundamental role in expanding the thoracic cage, during the respiratory acts - numerous nerve endings (intercostal nerves), arterial blood vessels and venous blood vessels.
What is intercostal neuralgia
Intercostal neuralgia is a rare morbid condition that occurs due to damage or malfunction of the intercostal nerves and is characterized by a characteristic intercostal pain.
Intercostal neuralgia is a form of neuropathic pain .
Intercostal nerves: where they originate and what they innervate
The intercostal nerves are peripheral nerves (that is, belonging to the peripheral nervous system ), which originate from the spinal cord .
Their main function is to innervate the muscles of the thoracic cage, the skin that covers the thorax and the tissues of the thoracic cavity.
WHAT IS NEUROPATHIC PAIN?
Neuropathic pain or neuralgia is a painful sensation that appears following a deterioration, or a malfunction, of the nerves of the peripheral nervous system (peripheral neuropathic pain) or of the structures of the central nervous system (central neuropathic pain).

Image from: www.clinicalexams.co.uk
Neuralgia is a different kind of pain than an individual feels after a wound, a burn, a compression or a trauma. In fact, in these second circumstances, the painful signaling starts from cutaneous receptors - called nociceptive receptors - which send messages from the periphery to the central nervous system, informing the latter of something abnormal and dangerous for the organism.
The painful stimulus produced by nociceptive receptors is called nociceptive pain and, unlike neuropathic pain, is an easier problem to interpret, from the aspect of the causes, and above all to cure.
Causes
Intercostal neuralgia can arise for a variety of reasons.
Possible causes include:
- Surgery in the heart or lungs, involving one or more incisions in the chest . In performing these incisions, in fact, the doctor could damage the intercostal nerves and cause them to malfunction. In this regard, readers are reminded that a nerve (or any other nervous structure), once damaged, is substantially irreparable.
Surgery involving the incision of the chest is at the origin of most cases of intercostal neuralgia, therefore they represent the most important cause.
- The compression of one or more intercostal nerves . To compress (or crush) the intercostal nerve endings can be a surrounding inflamed tissue or the cell mass of a tumor.
The compression of the intercostal nerves is a real pathology, forming part of the so-called nerve compression syndromes.
- An intercostal neuritis . Neurite is the medical term used to indicate inflammation of one or more nerves. The inflammatory process that leads to the onset of intercostal neurites generally originates at the level of the spinal cord.
If left untreated, inflammation of a nerve can cause it to be damaged.
- Chest traumas, which damage the intercostal nerves . Strong strokes to the rib cage can damage the intercostal nerve endings, fracture one or more ribs and cause respiratory problems.
Traumas that can determine these consequences are those that can occur during contact sports (such as rugby, football, American football, ice hockey, etc.) or at the time of a car accident.
- The state of pregnancy . With the enlargement of the fetus, the expansion capacity of the rib cage changes and this can temporarily alter the normal functioning of the intercostal nerve endings.
- Rib infections . They fall into the category of osteomyelitis, that is, infectious bone diseases, sustained by bacteria.
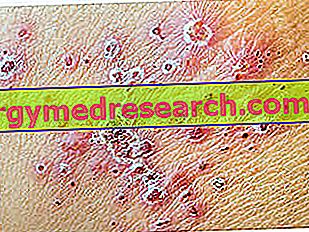
- Herpes zoster infections . Herpes zoster is the virus that causes shingles and chickenpox in children.
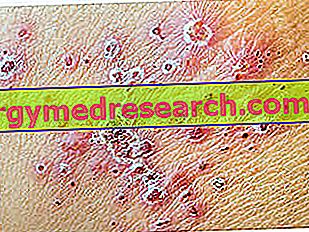
Doctors define this painful sensation with the term post-herpetic neuralgia, while they call the condition in which Herpes zoster is hidden within the nervous structures with the word latency.
RISK FACTORS
All those who are particularly at risk of intercostal neuralgia:
- They must undergo heart or lung surgery.
- They contracted the Herpes zoster virus.
- They practice contact sports, such as football players, rugby players, American football players etc.
- They have been involved in motor vehicle accidents and have received a severe blow to the chest.
Symptoms and Complications
The symptom that characterizes intercostal neuralgia is intercostal pain .
This painful sensation can be acute and episodic or deaf and constant.
When it is acute and episodic, patients compare it to a stabbing; while when it is deaf and persistent, they describe it as something slightly rodent or lacerating.
The intensity of the pain can increase, sometimes even markedly, following: deep breaths, lifting weights, coughing, sneezing, loud laughter, intense exercise and torsion / bending of the bust.
LESS COMMON SYMPTOMS
Depending on the triggering cause, intercostal neuralgia can also determine the presence of:
- Abdominal and / or lumbar pain
- Widespread pain in the chest, left arm and left shoulder. Remember the painful sensation that characterizes the heart attack (myocardial infarction) or angina pectoris; therefore, on first examination the doctor may not understand the exact nature of the symptomatology in progress.
- Loss of appetite
- Temperature. It is a classic sign of infections.
- Itch. It characterizes the cases sustained by Herpes zoster.
- Tingling and numbness. They are two typical manifestations of intercostal nerve compression or damage to them.
- Reduced motor capacity of the shoulders and / or back.
COMPLICATIONS
Premise: addressing a discussion concerning the complications of intercostal neuralgia is quite complex. In fact, it would also be necessary to consider the triggering causes and what they imply in the absence of adequate treatment or a late diagnosis.
A strong intercostal pain can represent an obstacle to breathing, especially the deep one.
Failure to breathe deeply can lead to the appearance of pneumonia and various types of lung infections .
Breathing difficulties and their consequences are probably the complications common to almost all forms of intercostal neuralgia.
WHEN TO REFER TO THE DOCTOR?
Any intercostal pain with the aforementioned characteristics or for which particular triggering causes are suspected deserves medical consultation.
Moreover, as we have seen above, numerous morbid conditions can hide behind intercostal pain, some of which are also very serious (a tumor, a bacterial / viral infection, a heart problem, etc.).
Diagnosis
To establish whether a given symptomatology is referable or not to an intercostal neuralgia, the objective examination, including a neurological evaluation, and some instrumental tests are fundamental.
If the former is important because it provides useful information on the current morbid condition and possible causes, the latter serve mainly to exclude pathologies with symptoms similar to intercostal neuralgia ( differential diagnosis ).
EXAMINATION OBJECTIVE
A thorough physical examination requires the doctor to visit the patient, looking for any clinical signs on the latter (swelling, bruising at the thoracic level, etc.), and discuss it about the symptoms.
Typical questions are:
- What is the pain? Is it accompanied by any other symptoms (fever, itching, abdominal pain, back pain, etc.)?
- When did the painful sensation appear? Is there any particular event at its origin (trauma, surgery, infection with shingles, etc.)?
- What movements or gestures enhance the symptoms?
Generally, after this first phase, the examination ends with: palpation of the painful area (to understand whether the compression causes pain or not), the auscultation of the lungs and the heart (in search of any abnormal sounds), some neurological evaluation tests and analysis of the head, neck, spinal cord and belly.
Importance of clinical history
When, from the evaluation of the history, it emerges that the patient has recently undergone a chest surgery or has suffered from Herpes zoster, the diagnosis of intercostal neuralgia is quite simple and immediate.
INSTRUMENTAL TESTS
The instrumental exams that allow further clarification of the situation, where doubts remain, are:
- Chest radiograph (Rx-thorax)
- TAC (Computerized Axial Tomography)
- Nuclear magnetic resonance (RMN)
- The electrocardiogram
Rx-thorax, CT and MRI provide images of the thoracic organs and the various skeletal, muscular and articular structures of the thorax.
The electrocardiogram, on the other hand, allows an evaluation of the cardiac activity and serves the doctor to make sure that the pain symptoms are not connected to some dysfunction of the heart.
Treatment
The therapy of intercostal neuralgia includes:
- The specific treatment of the cause that caused the damage or malfunction of the intercostal nerves.
- Pharmacological treatment of intercostal pain.
- Various physical (or non-pharmacological) treatments of symptoms.
Having said that, it is important to remind readers that some forms of intercostal neuralgia resolve spontaneously over time.
TREATMENT OF CAUSES
Acting on the triggering factors is, in many cases, fundamental to heal or, at least, to stop those processes that induce damage to the intercostal nerves. It is for this reason that, during the diagnostic process, the doctor emphasizes the search for the triggering causes and the events immediately preceding the onset of painful symptoms.
PHARMACOLOGICAL TREATMENTS
The drugs prescribed in the case of intercostal neuralgia include:
- Anesthetics for local use.
A widely used anesthetic, especially in the case of post-herpetic neuralgia, is lidocaine.
- Corticosteroids for local or systemic use .
Corticosteroids are powerful anti-inflammatory medicines which, if administered for long periods of time, can cause unpleasant side effects.
A highly used corticosteroid is prednisone.
- Tricyclic antidepressants .
Although it may seem strange, these drugs relieve neuropathic pain with a certain efficacy, and therefore also that which characterizes intercostal neuralgia.
Their effects are not immediate: for example, amitriptyline, which is the most administered tricyclic antidepressant in such situations, shows the first results only at the 2nd-3rd week of administration and the maximum therapeutic power at the 4th-6th.
Their incorrect and / or prolonged use has various side effects, including: drowsiness, dry mouth, decreased appetite, nausea and constipation.
- Non-steroidal anti-inflammatory drugs (NSAIDs) .
The most widely used NSAIDs are ibuprofen and aspirin. However, readers should be reminded that non-steroidal anti-inflammatory drugs have a very limited effect on neuropathic pain in general.
- Capsaicin in cream (therefore for local use) .
Capsaicin is a chemical compound found in hot pepper plants, which somehow manages to stop the painful signal sent from nerves to the brain.
- Opioid-type painkillers (or opiates) .
Opioid-type painkillers are derived from morphine and are among the most important pain medications.
Unfortunately, if used for long treatments or in excessive doses, they can be very dangerous.
The most used opiates in the presence of intercostal neuralgia are oxycodone and tramadol.
For doctors, the thorniest problem in prescribing some of the aforementioned drugs (in this case corticosteroids, opiates and tricyclic antidepressants) lies in the quantification of the most appropriate dose. By the most appropriate dose is meant, in this case, the minimum amount of effective drug.
Since each patient represents a case in itself, doctors establish the most appropriate doses only after several attempts.
PHYSICAL TREATMENTS
Physical treatments and TENS ( Transcutaneous Electric Nerve Stimulation ) are the physical treatments that are effective in alleviating the painful sensation.
Physiotherapy exercises consist mainly of stretching the intercostal muscles and the bust in general.
TENS, on the other hand, is a particular medical technique, which involves the infusion of some electrical discharges aimed at reducing the transmission of painful signals. Electrical discharges originate from electrodes, similar to patches to be applied to the skin.
Prognosis
The prognosis varies from patient to patient, depending on the factors triggering intercostal neuralgia.
In fact, if the causes are treatable (or can be resolved with time), there are more than fair chances of recovery; if instead the causes are not treatable (for example, a nerve damage following a surgical intervention), the only solution consists in the symptomatic therapy of alleviation of pain.
Prevention
Wear the appropriate sports equipment, drive carefully, fasten your seat belt in your car and get vaccinated against the herpes zoster virus (indicated above all for people over the age of 60) are the four behaviors recommended by doctors when they talk about prevention of intercostal neuralgia.