Generality
Electromyography is a diagnostic test that allows to study how the motor neurons of a specific area of the body interact with the muscles connected to them.

To perform electromyography, surface electrodes, needle electrodes and a recording device called an electromyograph are required.
Low-risk procedure, electromyography is contraindicated for people with an implantable pacemaker or cardioverter-defibrillator, and for those suffering from haemophilia or lymphedema.
The exam can last from 30 to 60 minutes.
What is electromyography?
Electromyography is a diagnostic procedure aimed at assessing the state of health of the muscles and cells that control the latter, or the so-called motoneurons .
From the instrumental point of view, it involves the use of some electrodes and a particular computerized apparatus (the electromyograph ), capable of recording the nerve signals that travel through the motor neurons and reach the muscles. All this is transformed into a graph that, once the diagnostic examination is completed, will be interpreted by a doctor.
MOTONEURONI: SHORT REVIEW
Since they have been named several times, it is wise to briefly review what motor neurons are.
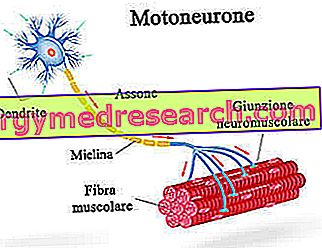
Motor neurons, or motor neurons, are cells that originate in the central nervous system (brain and spinal cord). Their function is to conduct nerve signals that directly or indirectly control muscles and muscle movements. In fact, thanks to the extensions they possess (NB: axons), the motor neurons reach the peripheral areas of the body.
There are two types of motor neurons :
- Somatic motoneurons (or somatic motor neurons), which directly innervate skeletal muscles;
- Visceral motoneurons ( visceral effector neurons), which indirectly innervate glands, heart and smooth muscles.
- the soma (or cellular body), which, located at the level of the gray substance, is the area containing the nucleus and the organelles, typical of any cell;
- the dendrites, which are the branches responsible for receiving the incoming nervous signals and leading them to the soma;
- the axon, which is a sort of long extension having the task of transmitting the nerve signal from the soma (central nervous system) to the periphery (the muscles).
WHO EXECUTES THE EXAM
Usually, it is a medical staff technician who performs electromyography, while a neurologist is to interpret the results of the procedure.
Neurologists are medical internists who specialize in the diagnosis and treatment of diseases that can affect the brain, spinal cord, nerves and muscles.
When you run
Doctors use electromyography when their patient complains of one of the following symptoms or signs:
- Tingling
- Muscle weakness
- Numbness
- Muscle pain or cramps
- Paralysis
- Involuntary muscle spasms
These disorders can be the manifestations of different pathologies, some even very serious, such as:
- Muscular diseases.
They are morbid conditions characterized by the presence of alterations of muscle fibers. Muscular dystrophies and myositis (polymyositis in particular) are a classic example.
- Diseases that impair the ability of motor neurons to communicate with the muscles to which they are connected.
Among these pathologies, the best known is myasthenia gravis, a chronic condition with autoimmune origin that causes mainly muscle weakness.
- Peripheral nerve diseases.
Peripheral nerves are all nerve cells that do not reside in the central nervous system.
Carpal tunnel syndrome and so-called peripheral neuropathies are a classic example of peripheral nerve diseases.
- Motor neuron diseases located in the brain and spinal cord.
If in the case of myasthenia gravis (and the like) the muscle cells with which the motor neurons communicate are altered, in these pathologies the motor neurons themselves deteriorate progressively until death.
The most well-known motor neuron diseases are ALS (also called amyotrophic lateral sclerosis or Gehrig's disease ) and poliomyelitis .
- Diseases that affect the nerve root.
A classic example of these conditions is the herniated disc .
Preparation
People with a pacemaker or an implantable cardioverter defibrillator, and those who suffer from a coagulation disorder (such as haemophilia) or lymphedema, cannot undergo electromyography. Therefore, those who fall into one of these categories of patients must notify the attending physician, to avoid complications during the procedure.

Figure: Carpal tunnel syndrome
It is also important to report to the neurologist, who will carry out the examination, which drugs are being taken, especially if among these there are anticoagulants (blood thinners).
IF THE PATIENT IS SUITABLE FOR THE EXAMINATION
Patients who do not have any contraindication to electromyography must follow these simple preparatory indications:
- If you are a smoker, do not smoke in the three hours before the exam.
- Take a full shower to remove any skin oils or creams from the skin. After showering, of course, no skin lotion should be applied, whether it has an aesthetic purpose or a therapeutic purpose.
- Do not wear tight-fitting clothing in the area of the body where the examination will take place, as they may be disturbing.
MEETING WITH THE DOCTOR
Generally, a few days before electromyography, the neurologist meets the patient to explain to him what the whole procedure consists of, what the possible risks are and what indications to follow on the day of the exam.
It is at this time that, if the patient has doubts or fears, he must ask all the appropriate questions.
Procedure
During an electromyography, the patient is seated in a chair or on a couch, so that he feels more at ease.
The exam usually includes two phases or moments:
- a first phase dedicated to the study of the conduction of nerve signals along the affected area;
- a second phase dedicated to the evaluation of the electrical activity of the muscle or muscles, located in the painful anatomical area.
Complete electromyography - where the first and second phases are understood to be complete - can last up to 60 minutes .
An electromyography that ends with the first moment, on the other hand, can be completed in about 30 minutes.
NERVOUS CONDUCTION STUDY
During the study of nerve conduction, the neurologist uses electrodes applicable to the skin surface for two purposes:
- Understanding the magnitude of the nerve signal that runs through the motor neurons innervating the symptomatic area. This signal is transferred to the electromyograph, to which the electrodes are connected, whose function is to transform the nerve signals into graphic signals.
- Release very mild electrical stimuli (NB: an electrical stimulus is comparable to a nervous stimulus). The release of small stimulations allows to test how the motor neurons interact with the muscles of the symptomatic area, when the nervous signal that passes through them undergoes variations.
Clearly, for each different stimulus, the electromyograph constructs a different graph, which only an expert is able to decipher correctly.
Sensations felt by the patient
In some cases, the release of electrical stimuli can create unpleasant sensations, similar to painful pangs or spasms. However, it should be noted that they are very short and have no repercussions on the health of the individual under examination.
EVALUATION OF MUSCULAR ELECTRICAL ACTIVITY
During the evaluation of electrical muscle activity, the neurologist uses needle electrodes (at least five), capable of recording the electrical activity of the muscle or muscles in which they are inserted.
The recording takes place both when the or the muscles of the symptomatic zone are at rest, and when they are under contraction; this double measurement is essential to catch any anomalies.
As in the case of nerve conduction, the instrument that plots the electrical activity is always the electromyograph.
Sensations felt by the patient
The insertion of the needle electrodes causes pain, as the skin is perforated. However, the wounds that are created are really limited in size.
risks
Electromyography is a low-risk diagnostic procedure, especially if all the preparatory indications have been followed.
In those rare circumstances in which problems arise, these may consist of:
- A few days lasting soreness at the area where the electrodes were applied. In such situations, doctors advise taking a mild anti-inflammatory (or a mild painkiller), to reduce the painful sensation.
- Tingling, hematoma and swelling where the needle electrodes are inserted. If these disorders worsen rather than improve, you should contact your doctor immediately, because it could mean that an infection is in progress.
- Damage, during the insertion of the needle electrodes, of the nerve endings that connect to the analyzed muscle or muscles.
- If the affected area is the thorax, the insertion of a needle electrode could cause air to penetrate between the lung and the pleural space and cause a pneumothorax.
Results
Usually, neurologists analyze the results of electromyography immediately, so as to discuss it immediately with the patient.