What is acute pyelonephritis
Acute pyelonephritis is an infection of the renal pelvis and interstitial tissue of the kidney, with rapid onset, which generally affects young women.

The pathology requires immediate intervention: if not treated properly, acute pyelonephritis can cause permanent damage to the organ and bacteria can spread to the bloodstream causing an infection spreading to the entire body.
Treatment of acute pyelonephritis includes antibiotic therapy and often requires hospitalization.
Diagnosis
The diagnosis of acute pyelonephritis is not always simple: there are differences in the clinical presentation and in the severity of the disease, in fact there is no coherent set of signs and symptoms that allows to identify the pathology in a specific way (the symptoms could also be linked to other infections urinary tract, such as cystitis or urethritis).
In the outpatient setting, the formulation of the diagnosis of acute pyelonephritis usually begins with the collection of information relating to the patient's clinical history, with medical history and physical examination, and is confirmed by the results of urinalysis, which should include microscopic analyzes. Other laboratory investigations are used to identify the occurrence of secondary complications. In general, imaging studies are used in the following cases: suspected subclinical presentation of the disease, atypical or insidious onset disease (gradual and usually associated with poor prognosis), resistance to therapy, need to quickly diagnose the occurrence of severe secondary complications (kidney stones, obstructive uropathy, perirenal abscess, etc.).
For this series of reasons, doctors must maintain a high suspicion index.
The presence of a symptomatology, characteristic of an infectious process, can orient the diagnosis: | |
CLEAR symptoms, indicative of acute pyelonephritis | High fever, lumbar pain, dysuria and renal involvement on physical examination. |
Some symptoms that can cause DIAGNOSTIC UNCERTAINTY | The appearance of infection at the kidney level sometimes occurs in the child only with the appearance of fever, but is often associated with loss of appetite, abdominal pain, fatigue and foul-smelling urine. In the elderly patient, the only symptom may be a vague feeling of discomfort. |
The microbiological investigation (microbiological culture of urine + direct microscopic examination) confirms the clinical suspicion in all these cases. | |
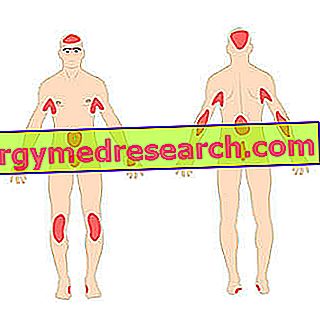
Physical examination
Your doctor may suspect that a kidney infection is in progress by performing a complete physical examination. The evaluation includes the control of clinical parameters, such as: heart rate, blood pressure, temperature control and any signs of dehydration. The patient suffering from acute pyelonephritis commonly presents lower back pain (at the level of one or both kidneys), which is manifested by a marked sensitivity of the kidney to palpation. If the affected person is a young woman, a pelvic exam may also be useful.
Laboratory investigations
Urinalysis : direct microscopy and microbiological culture
Microbiological diagnosis is a fundamental tool for providing a direct diagnosis.
Urine is the typical sample in which the etiological agent of acute pyelonephritis is sought and must be subjected to analysis by microscopy and culture, even in the case of a poor correlation between symptoms and bacteriuria. The urine culture must also be included in the "screening" of high-risk patients, such as pregnant women, the elderly, catheter-carrying patients, subjects with anatomic-functional alterations of the urinary tract and in all cases of sepsis of unknown origin . We also remind you that the presence of bacteria in the urine (bacteriuria) can be "asymptomatic" and cause recurrence of the infection.
In order to obtain reliable results, the urine sample must be collected BEFORE THE BEGINNING OF ANTIBIOTIC THERAPY, suitably, so as not to suffer any contamination: in performing the extraction, using the technique of intermediate mite, catheterization or suprapubic puncture, one must take in consideration the presence of the bacterial flora resident in the urethra and in the adjacent zones.
Direct microscopy
The direct microscopic examination allows to analyze a drop of fresh urine, then let dry and processed with the Gram method (it allows to distinguish the Gram-positive bacteria, which retain the basic dye assuming a violet color, from the Gram-negative ones) .
The analysis of urinary sediment allows to highlight if there is a condition of pyuria (presence of purulent material in the urine), besides allowing the possible identification of leukocytes and their quantification ( leukocyte count ).
Quick urine test: dipstick
The test is performed by immersing the test strips directly in the urine sample.
The dipstick allows to carry out quickly some specific enzymatic tests, in order to highlight the enzymatic activity of leukocytes (esterases) and bacteria (nitrate-reductase, catalase, glucose-oxidase).
The test allows to test the sample for some parameters relevant for the diagnosis of acute pyelonephritis:
- Presence of nitrites, from the transformation of nitrates carried out by pathogenic germs (if positive, is dependent on the presence of an adequate microbial load).
- Leukocyte esterase (confirms the presence of white blood cells). A positive result indicates a possible urinary tract infection.
- Hematuria and proteinuria, in acute pyelonephritis are parameters present in modest quantities, but indicative of the presence of blood and protein in the urine.
Culture test
The urine sample is diluted and sown on culture media suitable for the growth of bacterial species which, with greater frequency, cause the onset of pyelonephritis; the procedure aims to determine the bacterial load (CFU / ml). The standard urine culture test is aimed at finding non-demanding microorganisms, such as enterobacteria, Gram-negative bacteria, Gram-positive bacteria, Staphylococcus spp ., Streptococcus spp. and yeasts. Specific microbiological analyzes allow, instead, to identify pathogens such as mycobacteria, anaerobic bacteria etc. A bacteriuria which is significant from culture, must be evaluated according to various conditions and interpreted according to the individual case.
In front of a positive urine culture, the antibiogram is associated , which allows to evaluate the sensitivity of the pathogens involved in the infection to the different antibiotics.
The culture of urine therefore assumes great importance, as it allows the isolation of the microorganism that causes the onset of acute pyelonephritis, confirms the diagnosis and facilitates the choice of adequate therapy based on the characteristics of the identified pathogen.
Visual exam
In the case of acute pyelonephritis, urine is often cloudy, due to the presence of purulent material.
The opaque appearance of the sample can be determined by the presence of erythrocytes, leukocytes, bacteria, epithelial cells or amorphous material.
Other tests can support the results:
- Antibody research : agglutination test for anti-enterobacterial antibodies. The presence of secretory type A (IgA) immunoglobulins is indicative of a local or recent local and infection response.
- PAR test (determination of residual antibacterial power): search for substances with antibacterial activity (usually certain drugs or chemotherapy).
Hematochemical examination
- Blood Culture . Positive in about 12-20% of patients with pyelonephritis.
- Blood count, with complete counts of blood cells and with particular interest in detecting neutrophil leukocytosis, typical of acute inflammatory processes.
- Inflammatory markers : presence of the reactive C protein, high sedimentation rate of erythrocytes (ESR).
- Procalcitonin . Recent studies identify it as a biological marker in the diagnosis of acute pyelonephritis in children younger than two years.
Farley test
The test is noteworthy as it is still present in scientific literature, however today it is little used since it requires a demanding maneuver with the introduction of a Farley catheter in an already infected urinary system:
- A urine sample is taken by catheter and is subjected to culture.
- The bladder is then emptied and treated with a solution containing an antibiotic and fibrinolytic enzymes.
- This solution is left in the bladder for 30 minutes to allow the elimination of the microbial load, before being emptied and washed with sterile saline.
- The physiological solution is eliminated from the bladder and 3 samples are taken, according to an interval of 10, 20 and 30 minutes.
If the infection affects the kidney, all the samples will be positive with a progressive increase in the titer (the bacterial charge will be present in the first sample taken, as in all subsequent samples).
Imaging
The diagnostic imaging is useful in case of clinical picture evidence, to confirm the diagnostic suspicion or the presence of structural problems. Imaging is mandatory in patients with recurrent pyelonephritis and can help identify possible obstructions (example: stones or stenosis).
Spiral computed tomography (CT) is the best investigation in adult patients and can be used to confirm the diagnosis. CT-spiral does not use contrast agents and reveals a moderate to severe pathological condition (as the milder cases may be "normal").
The ultrasound examination allows to identify abscesses, kidney stones or stenosis.
For children, the choice can be between an ultrasound and computerized tomography: CT is more sensitive, but the first is the safest option for the small patient (there is no exposure to radiation).
Currently, magnetic resonance imaging (MRI) is still a limited investigation, in the evaluation of acute pyelonephritis, for costs and availability. In adults, MRI can detect kidney infection, urinary tract obstruction, scarring, and help assess renal vasculature. Furthermore, magnetic resonance imaging, in the case of perirenal abscess, better defines the extent of pyelonephritis compared to computed tomography.
Renal scintigraphy with 99mTc-DMSA (radiopharmaceutical consisting of technetium + dimercaptosuccinic acid, which is localized at the level of the renal cortex) allows the detection of anatomical and functional abnormalities of the kidneys during acute pyelonephritis (example: scarring, distribution of real function, foci of infection ...).
Renal biopsy
Renal biopsy allows the identification of histological evidence of acute pyelonephritis and is occasionally used to rule out capillary necrosis or renal abscess formation.
Management of acute pyelonephritis
Conditions that require hospitalization
The serious conditions of acute pyelonephritis that require hospitalization are:
- pregnancy;
- diabetes;
- severe dehydration;
- signs of sepsis (example: tachycardia, tachypnea, hypotension, etc.);
- lack of response to primary care treatment;
- urinary tract obstruction;
- oliguria (decreased urinary excretion) or anuria (failure to release urine);
- suspicion of secondary complications;
- uncertain diagnosis;
- relapse of symptoms, as soon as antibiotic therapy has ended.