Generality
Dengue is an acute febrile disease, of viral origin, transmitted to humans through the bite of infected mosquitoes for having stung, in turn, a sick person.
The dengue virus is an arbovirus (a generic term referring to viruses transmitted to humans by arthropods), belonging to the genus Flavivirus and to the Flaviviridae family. To date, 4 different viral serotypes are known, among them very similar: DEN-1, DEN-2, DEN-3 and DEN-4, of which 2 and 3 are often associated with more serious forms of disease
Dengue can present in two distinct forms: classical dengue (benign form of the disease) and hemorrhagic dengue (DE, a severe and potentially lethal form), with or without a state of shock (SSD, dengue shock syndrome).
Contagion
As anticipated, the dengue virus is transmitted from human to human through the bite of mosquitoes - belonging to the genus Aedes (the same one that transmits to man the yellow fever), in particular Aedes aegypti - which have previously consumed a blood meal on a viremic host (found in the infectious period in which the Dengue virus circulates in the blood). In particular, the mosquito can transmit the virus after 1/3 weeks from the infecting meal.
Aedes mosquitoes, unlike the Anopheles (those that transmit malaria), bite during daylight hours, with a maximum of activity in the two hours after dawn and in the hours before sunset.
Direct infection from humans to humans, particularly rare, can occur only in the case of direct contact with the blood of the sick person during the viraemia phase (for example through transfusions). It is believed that the subject affected by dengue is infectious within 6 days (on average) following the onset of the disease.
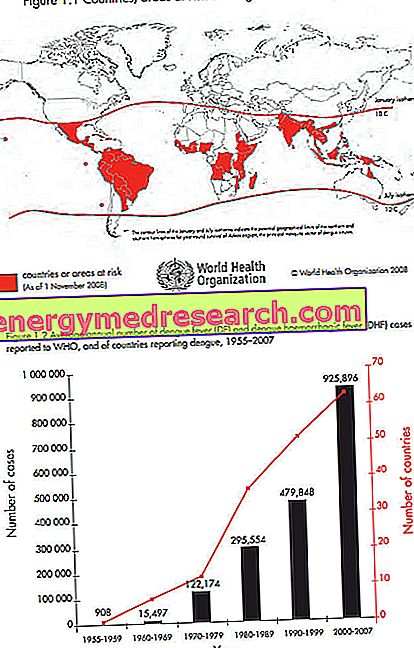
Epidemiology
Dengue is endemic in the tropical and subtropical areas, but it can also affect areas with a temperate-warm climate, where the so-called "import" forms are more likely: Tourists returning from endemic areas may indeed favor the sporadic spread of the disease in own country; in Italy, for example, Aedes mosquitoes, imported way back in 1990, are now widespread in at least 10 regions. Trade can also promote the spread of the disease outside the native areas; just think of the trade in used tires which, retaining small amounts of water inside, are the ideal habitat for mosquitoes to lay eggs.
Haemorrhagic dengue (ED) is particularly frequent in the regions of South-East Asia and the Pacific: it mainly affects children residing in these endemic areas, while it is rare in travelers.
Currently dengue fever is endemic in more than 100 countries, and its incidence in recent decades has increased considerably throughout the world. Around 50-100 million cases per year are included, including 500, 000 cases of ED and SSD, and 12, 500–25, 000 deaths (World Health Organization 2009). The peak of infections is recorded during and after the rainy season.
Symptoms
To learn more: Dengue symptoms
The incubation period can vary from 3 to 14 days, with an average of 5-7 days. Classical dengue initially manifests itself with symptoms that resemble those of a common flu form, heavier in children. After contracting and overcoming the infection, immunity generally lasts a lifetime but is highly serum-specific; this means that a subject immune to a serotype remains susceptible to other forms of Dengue (caused by the other three serotypes). In particular, the re-infection by heterologous serotypes in subjects immune to a serotype (even in the case of immunity acquired by the mother), increases the risk of developing the most severe form: hemorrhagic dengue.
The typical symptoms of classic dengue in the child include headache, even high and sudden fever, accompanied by chills, widespread prostration, and a maculo-papular rash (spots and bubbles not very prominent on the skin ) that recalls that typical of measles. In older boys and adults, classical dengue is a flu-like affection, with fever, headache, weakness, low back pain, osteo-articular and muscular pain (also called bone splitting fever), and gastrointestinal disorders, with or without the appearance of the above-described maculopapular exanthema (small red elements rash). The fever rise often seems to disappear after a few days, to then reappear later (saddle fever).
Hemorrhagic manifestations, typical of the most severe form of the disease, can sometimes also occur in classical Dengue, but in a much milder manner; the subject may, for example, complain of loss of blood from the nose and gums, notice blood in the eye (conjunctival haemorrhages), or suffer subcutaneous punctate hemorrhage (petechiae).
Hemorrhagic dengue (ED), more common in children under the age of 10-15, manifests itself in a two-stage pattern. In the first phase we witness the sudden onset of high fever (40-41 ° C) persistent, with reddening of the face, loss of appetite and slight disorders affecting the gastrointestinal tract and upper airways. This is followed by a period of weakness with a sense of well-being lasting about 24 hours, at the same time as the patient's condition may suddenly worsen, with the appearance of profound weakness, irritability, pallor, cyanotic color, especially around the mouth, lowering of pressure sanguine, rapid and weak pulse, rash. In this second phase there are frequent bleeding phenomena, from petechiae to ecchymoses (bleeding on the skin or mucous membranes, not detected, bluish or purple), epistaxis (loss of blood from the nose), blood loss from the gums, at bleeding of the gastrointestinal tract (presence of blood in vomit and faeces). Complications of the liver (hepatomegaly) and the central nervous system are possible. In severe cases, hypovolemic shock can occur due to the multiplicity and abundance of bleeding.
What to do in case of suspicious symptoms?
If the typical symptoms of the disease were felt when returning from a trip to endemic areas:
- Have a doctor visit you as soon as possible, in order to confirm the diagnosis and exclude diseases with similar manifestations, such as malaria, typhoid, yellow fever and other haemorrhagic fevers
- Rest and take plenty of fluids
- Eventually, in case of severe pain and headache, take an anti-inflammatory but avoid salicylates (Aspirin and the like), which can increase the risk of bleeding and cause Reye's syndrome in children.
Diagnosis
Considering the indistinguishability, on the symptomatological level, of classic non-exanthematic Dengue from other diseases accompanied by fever and flu-like symptoms, the diagnosis takes place through specific laboratory tests, aimed at finding specific antibodies, at identifying the virus's genetic material by PCR, or in search of alterations of the blood parameters typical of the disease.
Care and Treatment
To learn more: Drugs for Dengue Care
There is no specific treatment for the treatment of classical dengue; it is therefore suggested the generous intake of liquids and bed rest. The disease lasts on average 3-10 days and heals spontaneously, although the sense of weakness and prostration can accompany the patient even for several days or weeks after recovery. The possible pharmacological treatment is symptomatic: in case of high fever, antipyretics such as paracetamol and codeine can be used, while pain and itching can be attenuated by taking analgesics / anti-inflammatories (NSAIDs). Antipyretic and anti-inflammatory drugs based on acetylsalicylic acid (aspirin) must be avoided, which, by preventing normal blood coagulation, may favor or aggravate the appearance of hemorrhagic manifestations.
In dengue hemorrhagic the patient's conditions must be carefully controlled, correcting any dehydration (hypovolemia) and the electrolytic condition through specific intravenous infusions, in order to prevent the appearance of the shock. In extreme cases it may be necessary to transfuse blood, plasma or blood products.
Having contracted the disease confers immunity only for the virus that caused it; therefore, since dengue can be determined by 4 different serotypes of the virus, one can be infected again by one of the other three.
Prevention
Since there is not yet an effective vaccine, and it is not possible to implement a regimen of pharmacological prophylaxis as for malaria, it is fundamental to adopt measures aimed at eliminating or reducing mosquito infestation. These insects proliferate together with Dengue in tropical and subtropical regions, particularly in large urban and peripheral areas characterized by a high population density in areas, such as slums, where common sanitary regulations are absent or in any case poor (presence of sewage, unhealthy stagnant water, accumulation of solid urban waste). The preventive measures are therefore aimed at the adoption of a sanitary conduct that foresees the reclamation of these areas, through the prompt removal of solid urban waste, the correct removal and disposal of sewage water, periodic disinfestation interventions, and the elimination, especially near the houses, of the water collections that can be used for spawning and the development of larval forms. The application of mosquito nets and other protective devices to the windows of the houses is very useful.
At the individual level, the prevention of dengue is essentially based on avoiding being points
from mosquitoes, bearing in mind the "diurnal" habits of these insects (most active by day in the two hours accompanying the rising of the sun, and in the two hours preceding its sunset). In particular, the Ministry of Health recommends:
- wear light-colored clothes (dark and bright colors attract insects), with long sleeves and long trousers, which cover most of the body;
- avoid the use of perfumes (they could attract insects that transmit dengue);
- apply to the exposed skin insect repellents based on N, N-diethyl-n-toluamide or dimethylphthalate, repeating if necessary, for example in case of intense sweating, the application every 2-3 hours; insect repellents and pyrethroid-based insecticides can also be sprayed directly onto clothing;
- after a swim the repellent must be reapplied on the skin;
- preferably stay in rooms with air conditioner or, in the absence of this, mosquito nets on the windows, making sure that these are kept in order and well closed;
- spray insecticides based on pyrethrum or permethrin in living rooms and bedrooms, or use insecticide diffusers (operating with electricity or batteries), which contain tablets impregnated with pyrethroids (remember to replace exhausted plates) or coils pyrethrum mosquito repellent.
The possibility, especially in small children, of undesired effects of insect repellent products, imposes certain precautions in their use, and a scrupulous attention to the indications contained in the accompanying leaflets. In particular:
- the repellent product must be applied only on the exposed parts;
- it must not be inhaled or ingested, or brought into contact with the eyes;
- it must not be applied on irritated or excoriated skin;
- the application of highly concentrated products must be avoided, especially with regard to children;
- treated skin surfaces should be washed immediately after returning to closed rooms or when suspicious symptoms (itching, inflammation) occur, for which it is advisable to consult a doctor immediately