Generality
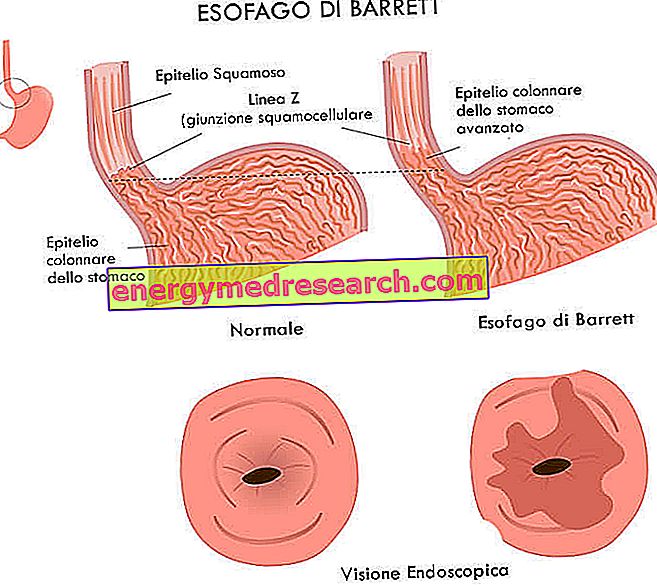
We talk about Barrett's esophagus when the normal tissue that covers this muscular conduit, located between the pharynx and the mouth of the stomach, is replaced with an epithelium similar to that which internally covers the walls of the duodenum (initial tract of the small intestine).

Causes
Barrett's esophagus is a typical complication of gastroesophageal reflux. Following the relaxation of the sphincter that virtually separates the esophagus from the stomach (called cardias), the ascent of the gastric juice into the esophagus determines - in the long run - a modification of the esophageal epithelium, which thus attempts to defend itself from the acid. The epithelial cells therefore take on characteristics very similar to those of the gastric or duodenal ones, characterizing the condition known as Barrett's esophagus. This complication is considered pre-cancerous, since the abnormal epithelium can undergo uncontrolled replication (cancer).
Data in hand, Barrett's esophagus is found in 15-20% of patients with chronic gastroesophageal reflux disease (GERD), especially in Caucasian men aged 50 or over.
According to recent epidemiological studies the risk of developing an adenocarcinoma in the presence of Barrett's esophagus can be estimated at 0.4 - 0.5% per year per patient, while the 5-year survival rate from the diagnosis of adenocarcinoma (cancer of the esophagus) it is very low (less than 10%). In light of these data, even if the risk is modest, it is desirable to carry out an endoscopic examination in all patients suffering from reflux, so as to exclude with certainty the presence of Barrett's esophagus.
POTENTIAL RISK FACTORS
- gastroesophageal reflux disease,
- hiatal hernia,
- overweight, c
- alcohol consumption
- smoke,
- male sex (men are twice as likely as women),
- Ethnicity: Caucasian,
- old age,
- familiar with Barrett's esophagus.
Symptoms
To learn more: Barrett's Esophagus Symptoms
Barrett's esophagus is an asymptomatic condition in itself, which, however, frequently accompanies the symptoms typical of the reflux disease that generated it (acid regurgitation, heartburn, difficulty swallowing food and pain in the stool; in the most serious cases notice blackish and tarry stools, and traces of blood in the vomit).
The severity of Barrett's esophagus does not depend so much on symptoms and related disorders, but on its potential evolution to adenocarcinoma (cancer of the esophagus).
Diagnosis
As anticipated, the diagnosis of Barrett's esophagus is based on the results of endoscopy and esophageal biopsy. A thin tube (endoscope), equipped with a light source and a camera at the end, is made to descend along the patient's throat, examining the state of health of the esophageal epithelium and searching for any metaplasias. In the event that these are present, using special instruments made to slide along the endoscope, the doctor takes small samples of abnormal tissue, which are subsequently examined microscopically by the expert pathologist. The report can therefore speak or not of dysplasia on metaplastic tissue and establish its severity (low grade or high grade) based on structural differences with the typical cells of the esophagus. The greater the dysplastic degree, the greater the risk of tumor evolution; for example, if dysplasia is particularly severe, the risk can rise up to 10% or more per patient per year. It should be remembered, however, that the dysplastic process is not a tumor process and can be reversible (while a transformed cancer cell can no longer return to normal).
Gastroesophageal reflux → esophagitis → Barrett's esophagus, metaplasia → dysplasia → adenocarcinoma
Treatment
Barrett's esophagus therapy must aim both at controlling the symptoms of gastroesophageal reflux and at healing esophagitis, but above all it must aim at restoring the normal esophageal squamous epithelium in areas of previous intestinal metaplasia. In this regard, so-called proton pump inhibitors are used, drugs capable of significantly reducing gastric acidity for a long time (18-24 hours). Although these medicines are very effective in eliminating the acid insult and cushioning symptoms associated with reflux disease, in many cases they fail to produce a significant regression of dysplastic tissue.
In the event that Barrett's esophagus is characterized by a low degree of dysplasia, the situation is monitored periodically through endoscopic examinations every 12-36 months. On the other hand, if there is a high degree of dysplasia, it may be necessary to remove or destroy the abnormal tissue (through special endoscopic instruments or with radiofrequency ablation or laser); the entire portion affected by Barrett's esophagus is much more rarely exported and in this case the residual tract is sewn up with the mouth of the stomach.