Generality
Renin is a proteolytic enzyme synthesized by the kidney. This protein is released in response to physiological stimuli, such as: decreased blood volume, hypotension and reduced sodium and potassium concentrations in the blood.

The blood dosage of renin, together with the measurement of aldosterone, is useful in the differential diagnosis of primary and secondary hyperaldosteronism.
What's this
Renin is an enzyme released by the kidney when the arterial pressure is reduced too much, and the organ is thus found to be in ischemic conditions.
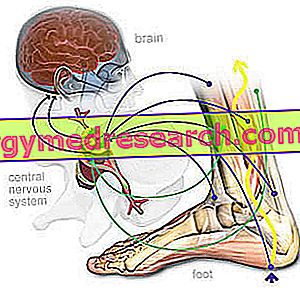
Being a proteolytic enzyme, renin is able to break down the peptide bonds present in other protein molecules; more precisely, it acts on angiotensinogen, an alpha2-globulin synthesized by the liver and normally present in the blood.
By renin intervention, angiotensinogen is converted to angiotensin I. In turn, this peptide undergoes a further enzymatic conversion originating angiotensin II (thanks to the intervention of the conversion enzyme - ACE).

Angiotensin I and angiotensin II are vasoactive molecules with hypertensive activity. They are therefore able to raise blood pressure, with a hypertensive action that reaches - as far as angiotensin is concerned - a force about 200 times higher than that of noradrenaline. This result underlies various biological mechanisms, ranging from the increase in the strength of cardiac contraction to the greater release of aldosterone, passing through a marked vasoconstrictor activity at the arteriolar level.
The aldosterone, produced by the adrenal cortex, stimulates sodium reabsorption, consequently increasing the plasma volume, arterial pressure and renal potassium excretion.
Renin is produced by a group of particular renal cells forming part of the so-called juxtaglomerular apparatus, therefore located in the walls of the arterioles afferent to the kidney.
Renin is not produced and secreted as such, but in the form of a precursor, pro-renin, which is decidedly more abundant in the bloodstream.
For the laws of homeostasis, renin release is stimulated by conditions of:
- Hypotension (low blood pressure values);
- Hypovolemia (reduced blood volume);
- Hyponatremia (reduced sodium concentrations in the blood);
- Hyperkalaemia (high concentrations of potassium in the blood).
Renin release is instead inhibited in diametrically opposed conditions.
More information on the renin-angiotensin system is presented in this article ..
Why do you measure
Plasma renin levels can be evaluated to investigate the origin of particular hypertensive forms, particularly when the levels of potassium in the blood are low.
Often, the dosage of renin is combined with that of aldosterone, given that - as explained in the previous paragraph - low levels of renin associated with high levels of aldosterone, or vice versa, may indicate the presence of a pathological condition (in healthy subjects when increases renin also increases aldosterone, and vice versa).
Aldosterone levels can also be measured in urine collected over a 24-hour period, thus benefiting from greater standardization (as aldosteronemia is influenced by the time of day and the body position assumed - orthostatism or posture).
Normal values
Under normal conditions, the following blood levels of renin are found:
- Orthostatism: 4.4 - 46.1 µIU / mL
- Clinostatism: 2.8 - 39.9 µIU / mL
Note : the reference interval of the exam can change according to age, sex and instrumentation used in the analysis laboratory. For this reason, it is preferable to consult the ranges listed directly on the report. It should also be remembered that the results of the analyzes must be assessed as a whole by the general practitioner who knows the patient's medical history.
High Renin - Causes
High renin in the blood can be the consequence of:
- Kidney diseases;
- Obstruction of the arteries that carry blood to one or both kidneys (see renal artery stenosis);
- Addison's disease;
- Hepatic cirrhosis;
- Hemorrhage;
- Renal-secreting renal and extrarenal tumors;
- Malignant hypertension;
- Congestive heart failure;
- Bartter syndrome (high renin levels without hypertension).
High levels of renin are also recorded in the case of:
- Dehydration;
- Hypokalemia;
- Low sodium diet;
- Loss of salts following gastrointestinal diseases (eg Diarrhea);
- Pregnancy;
- Taking contraceptive drugs containing estrogens or diuretics.
Low Renin - Causes
Low renin in the blood can be the consequence of:
- Conn syndrome;
- Cushing syndrome;
- Vasopressin (ADH) therapy or sodium-containing drugs.
How to measure it
To measure renin, the patient must have blood drawn from his arm; sometimes, a sample is collected from a renal or adrenal vein. The exam can also be performed on 24-hour urine.
Preparation
Before undergoing the renin test, it is necessary to observe a fast of at least 8 hours, during which a small quantity of water is allowed.
For the measurement on blood, the doctor may request the patient to stand in an upright position for at least an hour (renin in orthostatism) or supine for at least 2 hours (renin tilting).
Starting from two to four weeks before sampling, it is necessary to adopt dietary-behavioral measures to improve the diagnostic reliability of the test. In particular, at least two weeks before it is necessary to stop taking anti-hypertensive drugs (diuretics, beta blockers, ACE inhibitors), steroids, progestins and estrogens.
At the same time, the sources of caffeine and licorice should be removed from their diet, while the sodium intake should be maintained at reasonable and as constant as possible. A special diet, low in sodium, can be prescribed in the three days preceding the test, usually performed under fasting conditions for eight hours.
Interpretation of Results
The table below shows how the changes of renin, aldosterone and cortisol vary according to different pathologies (source Lab Test Online), indicating the need for a joint dosage in front of a clinical suspicion.
| pathology | Aldosterone | Cortisol | Renin |
| Primary hyperaldosteronism (Conn syndrome) | High | Normal | Bass |
| Secondary hyperaldosteronism | High | Normal | High |
| Cushing syndrome | Low-normal | High | Bass |
| Adrenal insufficiency (Addison's disease) | Bass | Bass | High |
| Pituitary disease | Normal | Bass | Normal |