Definition
Progressive ossifying fibrodysplasia (FOP) is a rare disease, characterized by the abnormal development of bone tissue in areas of the body where, as a rule, this is not present; the bone can form, for example, inside muscles, tendons, ligaments and other connective tissues.
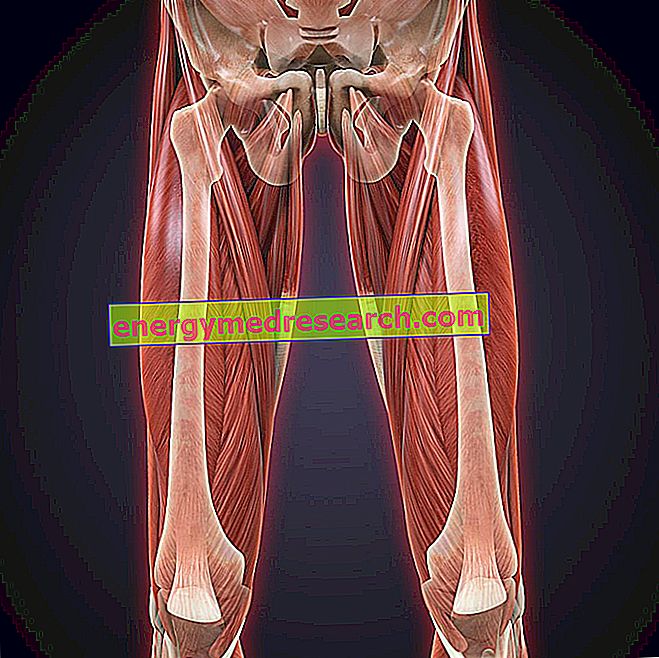
Bone formation outside the skeleton (a process defined as heterotopic ossification) progresses throughout the life of the affected individual; in many cases, the disease begins at the level of the neck and shoulders, therefore it extends along the back, the trunk and the limbs.
Progressive ossifying fibrodysplasia depends on mutations of one of the genes involved in skeletal formation during embryonic development and in its repair after birth.
The disease can be transmitted in an autosomal dominant manner, so a parent with the condition has a 50% chance of passing on the gene defect to each of their children. In most cases, however, progressive ossifying fibrodysplasia occurs sporadically, without involving other relatives, due to the appearance of a de novo mutation.
Most common symptoms and signs *
- asphyxiation
- Asthenia
- brachydactyly
- Dyspnoea
- Neck pain
- Shoulder pain
- Articolar pains
- Muscle pains
- Temperature
- Joint swelling
- Backache
- Nodule
- Joint stiffness
- Stiffness in the muscles of the back and neck
Further indications
Progressive ossifying fibrodysplasia usually occurs within 20 years of age. However, the first signs of illness can be observed already at birth and during childhood; in fact, the progressive ossifying fibrodysplasia is always associated, to the malformation of the toes (in particular, of the big toes), which can be short, bent and sometimes curved inwards.
In the early stages of the disease, episodes of acute inflammation may occur with soft tissue swelling. These inflammations can occur spontaneously or in response to particular stimuli (in general, trauma, but also infections, intramuscular injections or various types of injuries).
At the beginning, the affected areas can be reddened and sometimes painful and hot to the touch. Over time, swellings take on the consistency of fibrous nodules and, as the inflammation tends to resolve, they leave a new piece of mature bone in the area. Shoulders and backs are preferred for this event, but head, pelvis and limb roots can also be affected.

At the level of the joints, the progressive ossifying fibrodysplasia causes rigidity of the areas involved, associated with a more or less severe limitation of the movements. Over time, the formation of bone tissue in the muscles limits its functionality, to such an extent that the patient experiences blockage and permanent immobility (for example, the affected subject can no longer move his arms or walk).
In some cases, the ossification process is rapid and becomes unstoppable; in others, the course is more gradual and long periods can elapse between one episode and another. The involvement of the chest can trigger problems at the respiratory level, therefore inducing the patient's death due to complications such as pneumonia and asphyxia, on average around 40 years of age.
The diagnosis of progressive ossifying fibrodysplasia is based on clinical examination. The presence of heterotopic ossification can be evidenced through the execution of X-rays, while genetic tests allow to confirm the defect underlying the disease.
At the moment, there is no definitive treatment, but it is possible to reduce trauma and pain by taking NSAIDs and corticosteroids. In particular, the latter drugs, if administered within the first 24 hours following exacerbations, are able to counteract acute inflammation and bone formation, but without definitively blocking it.
Furthermore, in the presence of progressive ossifying fibrodisplasia, preventive interventions are necessary to reduce trauma (eg safety measures at home, use of a protective helmet, etc.) and to prevent respiratory dysfunction.