Generality
Newborn regurgitation is a condition that can occur in the first months of life .

The disorder manifests itself, in particular, when food, after feeding or eating, flows back from the stomach to the child's mouth. The result is the rejection of variable volumes of milk or other ingested foods. Newborn regurgitation episodes are typically preceded by irritability and crying .
In new parents, this phenomenon can cause some concern, but usually the phenomenon is transitory and tends to disappear with weaning (ie with the integration of solid foods in the child's diet).
Only in certain cases, the regurgitation of the newborn may depend on a more severe underlying pathology (eg gastroesophageal reflux disease, allergies and pyloric stenosis), which requires specific treatment.
What's this
Regurgitation is a common problem, as it affects at least half of children in the first 12-14 months of life. This consists in the return, from the stomach to the esophagus, of the food ingested with a feed or a meal.
Normally, newborn regurgitation is a temporary disorder and is a problem only when it prevents the child's correct growth; in this case, the situation must be assessed by a pediatrician.
Causes
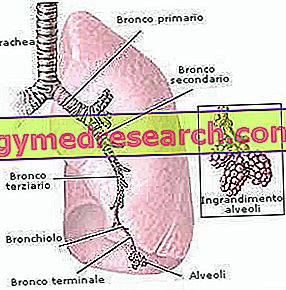
The regurgitation of the newborn is mainly caused by the immaturity of the cardia (or lower esophageal sphincter), ie the muscular ring located between the esophagus and the stomach, which regulates the unidirectional passage of food between these two organs.
As it is not yet fully developed in very young children, this structure is incontinent and can cause the material in the stomach (food or gastric juices) to flow back.
Usually, newborn regurgitation tends to disappear with weaning. It is unlikely that the disorder will occur after 18 months.
Possible diseases associated with newborn regurgitation
The regurgitation of the persistent newborn or associated with severe symptoms (weight loss, recurrent crying, repulsion for food, violent vomiting or with traces of blood, etc.) may indicate an underlying pathological condition, including:
- Pyloric stenosis : consists in the narrowing of the sphincter placed between the stomach and the duodenum ; this prevents the complete passage of food from the stomach to the intestine, that is the complete gastric emptying;
- Food intolerance : it occurs mainly against some cow's milk proteins, used instead of the maternal one.
Less frequently, newborn regurgitation is the indicator of more complex diseases, such as:
- Allergy ;
- Eosinophilic esophagitis (inflammation of the esophagus supported by an allergic-type reaction, in which there is a high presence of eosinophils);
- Obstruction or narrowing of a tract of the digestive tract.
When inflammatory lesions of the esophagus are associated with newborn regurgitation, a gastroesophageal reflux disease may be present. This means that the rise of food and gastric juices in the stomach is a constant and not sporadic phenomenon. In children, gastroesophageal reflux disease depends above all on a marked immaturity of the cardia and is observed more frequently in the case of premature birth, milk allergy or muscular and / or neurological diseases (as happens, for example, in the case of cerebral palsy) .
Risk factors
Newborn regurgitation may arise due to a combination of common factors, which are often difficult to avoid.
The disturbance may simply depend on the fact that the air that the newborn swallows by sucking the milk remains trapped in the liquid; when the child feels the need to expel it, the liquid is also regurgitated.
Sometimes, reflux occurs when the newborn is particularly voracious or tends to eat more than necessary.
The elements that may affect the appearance of the problem therefore include:
- The extended stay in a relaxed position;
- The almost entirely liquid diet, typical of the neonatal age;
- Excessive speed in drinking by the child;
- The amount of food given to the newborn;
- The formation of air bubbles in the stomach that push the food present towards the esophagus.
Symptoms and Complications
Generally, the regurgitation of the newborn does not cause particular problems to the child and only in rare cases should be a real cause for concern on the part of the parents.
The disorder can manifest itself with small emissions from the mouth of the food previously ingested, a sign indicating the rise of the gastric contents towards the esophagus.
Other symptoms may also be associated with the newborn's regurgitation, such as:
- Inappetence (poor appetite, often accompanied by a sense of repulsion for food);
- Frequent plants, especially after meals and at night, when the child is lying down;
- Irritability .
Vomiting can also be added to regurgitation, but it is a more rare phenomenon.

When it depends on another pathology
If the regurgitation of the newborn is caused by a more serious pathology (such as, for example, an allergy or gastroesophageal reflux disease), there may be signs of poor development (or slowing of growth) associated with:
- Refusal or difficulty in eating;
- Weeping during the meal or after eating;
- Decrease in body weight;
- Frequent cough;
- Hiccup;
- Recurrent eruptions.
In children suffering from gastroesophageal reflux disease, chronic respiratory manifestations such as:
- Recurrent laryngitis;
- Asthma;
- Otitis media;
- Night cough.
Possible consequences
- Some scientific researches have hypothesized that frequent episodes of regurgitation in the neonatal age may predispose to the development of gastro-esophageal reflux disease during late childhood.
- Aspiration of gastric material into the airways secondary to newborn regurgitation may be responsible for recurrent pneumonias. The acute onset of fever, cough, dyspnea and rales suggests the possibility of aspiration pneumonia .
When to consult a doctor
Newborn regurgitation is a condition that, in mild form, occurs quite frequently, therefore it is considered a nearly normal phenomenon.
However, it is advisable to consult the pediatrician if the child manifests:
- Weight loss or loss of weight;
- Green or yellowish regurgitation;
- Vomit with traces of blood or dark colored material (similar to coffee grounds)
- Strong repulsion for food;
- Blood in the stool;
- Breathing difficulties or chronic cough.
It is always advisable to contact the pediatrician for any doubts but, in particular, in the presence of one or more of the symptoms listed, to investigate the situation.
Diagnosis
To assess the extent of regurgitation of the newborn (ie whether or not it is a serious problem), the pediatrician must perform a thorough physical examination, during which he visits the child and questions the parents about the symptoms or signs noted up to that point.
If the newborn showing sporadic episodes of regurgitation is in good health, grows as it should and looks healthy, no other special diagnostic investigations are necessary.
On the contrary, further checks could include:
- Ultrasound : it is used to clarify if the child suffers from pyloric stenosis;
- Laboratory tests: blood and urine tests can help to clarify the possible causes of recurrent vomiting and poor weight gain. These investigations are also useful for the purposes of a differential diagnosis (that is, when evaluating any conditions that arise with symptoms similar to the suspected one);
- Esophageal pH monitoring : by means of esophageal ph-metrics, the acidity of the tract under examination is measured;
- Radiography : they are useful in identifying alterations of the gastrointestinal tract, such as, for example, an obstruction;
- Endoscopy of the upper digestive tract : involves the observation of the inner walls of the esophagus, the stomach and the initial part of the intestine, by means of an instrument called an endoscope; this exam is useful to highlight the presence of narrowing or inflammatory states (eg esophagitis). Furthermore, during endoscopy, tissue samples (biopsy) can be collected for histological examination.
Treatment and Remedies
Remedies against Newborn Regurgitation
As anticipated, the regurgitation of the newborn tends to resolve spontaneously with weaning.
In the meantime, however, the pediatrician may recommend simple steps:
- Administer small meals (ie with small amounts of milk or food), but more frequent;
- Give the baby small bites and moderate the speed of food delivery;
- Hold the baby in his arms for 20-30 minutes after a meal, preferably in a vertical position, to allow him to burp;
- Avoid lying down immediately after eating or feeding;
- Eliminate dairy products, beef or eggs from the mother's diet during breastfeeding, to check if the baby has an intolerance;
- Use a different teat size for the bottle. A teat that is too wide or too narrow can cause the baby to swallow air.
When these remedies are ineffective or if the presence of a cow's milk allergy or a gastroesophageal reflux disease is confirmed, it is necessary to resort to specific and targeted therapies.
drugs
In case of regurgitation of the newborn, drugs are generally not recommended: anti-reflux medicines can interfere with the absorption of calcium and iron, in addition to increasing the risk of intestinal infections. Despite these considerations, the physician can prescribe drugs that can reduce acid production by the stomach, such as omeprazole (proton pump inhibitor) and / or ranitidine (histamine H2 receptor antagonist). Usually, anti-acid medicines are indicated only if strictly necessary, ie if the child does not gain weight, regurgitation is chronic and conservative remedies do not limit the problem.
Surgery
As for surgery, this is considered in very rare cases of newborn regurgitation. Usually, the intervention is carried out at the level of the cardia, in order to offer greater resistance to rising food upwards.
The lower esophageal sphincter is treated with a Nissen-Rossetti fundoplication procedure only when the regurgitation is so severe that it prevents the normal development of the newborn or compromises normal breathing.