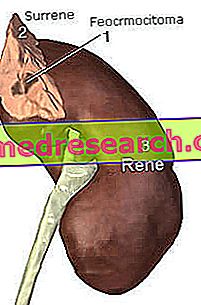
What is pheochromocytoma
Pheochromicitoma is a tumor that develops in the adrenal gland, generally affecting its innermost portion, called medulla, where chromaffin cells are found. It is a rather rare neoplasm, with an estimated incidence between 2 and 8 cases per million inhabitants; pheochromocytoma recognizes a certain family predisposition and is more common among young adults and in middle age groups.
Adrenal glands and catecholamines
The adrenal glands, placed like a hat over the kidneys, produce in their central portion two very important hormones, respectively called adrenaline and noradrenaline, or more generally catecholamines. Together, they regulate the body's response to psychophysical stress, preparing it for the so-called attack and flight reaction. In such circumstances, thanks to the massive secretion of these hormones, the heart increases the strength and the contractile frequency, the bronchi, the pupil and the blood vessels of the appendicular and coronary system dilate, while at the liver level the glycogenolysis is stimulated.
At the same time, again with the aim of preparing the body for impending physical activity, the digestive processes are significantly slowed down, while the cutaneous and peripheral blood vessels become constricted and the arterial pressure increases; the bladder relaxes, while the urethral sphincter narrows (inhibits urination).
Symptoms
To learn more: Pheochromocytoma symptoms
Since pheochromocytoma is a catecholamine-secreting tumor, it is very often accompanied by hypertension (fundamental clinical manifestation) and symptoms such as sudden headaches, pallor, profuse sweating, chest pain, weight loss, nervousness, anxiety, anxiety, tremors, palpitations and sensation of more energetic heart beat. Sometimes it can be asymptomatic.
Sometimes the symptoms of pheochromicotoma include gastrointestinal disorders, such as abdominal pain, nausea and vomiting, and alterations of glucose metabolism, such as reduced glucose tolerance or a diabetes free.
In relation to the release of catecholamines from the tumor, the symptomatology can occur in an accessory way (sudden and violent attacks, lasting less than an hour) or continuous. Furthermore, the consequences of arterial hypertension on target organs (eg retinal problems) can be added to all these symptoms.
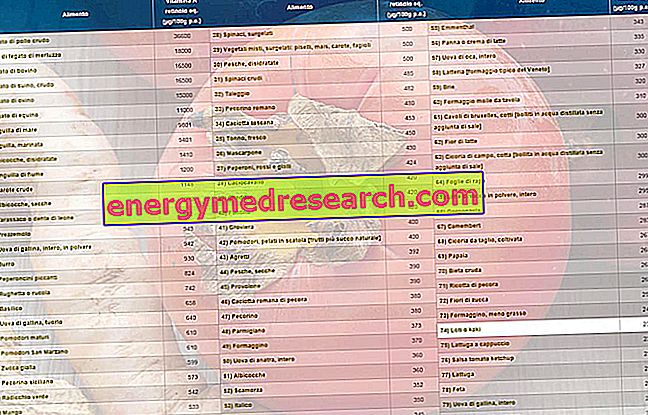
The symptoms of pheochromocytoma can suddenly worsen giving rise to hypertensive crises; this happens above all following emotional stress or anxiety, surgical anesthesia or physical efforts that cause a certain pressure on the tumor (changes in position, sporting activity, diagnostic maneuvers (catheterization), lifting of a weight, defecation, urination, pregnancy, etc.) . The symptoms of the pheomocrocytoma can also be exacerbated by the use of some drugs, drugs (amphetamines, high-dose caffeine, ephedrine, decongestants, antihistamines, cocaine, etc.) and foods (those rich in tyramine), which raise blood pressure. The use of metoclopramide, atropine and MAO inhibitory drugs (risk of hypertensive crises with cardiac damage) should also be avoided in the presence of pheochromycoma; among the latter we mention isocarbossazide, phenelzine, selegiline, moclobemide and tranylcypromine. Hypertensive crises can be controlled with drugs such as nitroglycerin and derivatives.
Diagnosis
See also: Urinary Metanephrine
The diagnosis of pheochromocytoma is based on the dosage of adrenaline and noradrenaline, and of the related metabolites (metanephrines), in blood and urine. If the levels are high, the exact localization of the pheochromocytoma is detected by a CT scan, an abdominal magnetic resonance, a PET with 6- (18F) fluorodopamine, or through a scintigrafia with meta-iodobenzilguanidina (MIBG) or with marked analogues of somatostatin (octreoscan).
Treatment
The treatment of choice, when practicable, is surgical.
In fact, with the removal of the adrenal gland affected by the pheochromocytoma, the symptoms tend to disappear in most cases; cardiac pressure also returns to normal. If the neoplasms involve both glands, it is therefore necessary to remove both adrenals; unfortunately, bilateral adrenalectomy requires chronic replacement therapy to replace the various adrenal hormones, such as cortisol and aldosterone.
When possible, surgery is performed laparoscopically, that is by inserting thin precision instruments into small incisions made in the patient's abdomen.
Indispensable, pending the intervention and in preparation for it, the intake of alpha and beta blockers and, if necessary, of other drugs to control blood pressure and the various symptoms triggered by pheochromocytoma.