Generality
Rubella is a contagious disease, typical of childhood and caused by a viral infectious agent (ie a virus) known as rubella virus .

The typical rash of rubella.
From wikipedia.org
Its onset usually involves: the appearance of numerous red skin spots (skin rash), the enlargement of some lymph nodes located near the neck and ears and, finally, the classic symptoms of a cold.
When rubella affects adults and pregnant women, especially in the latter, it can give rise to serious complications.
Currently, there is no specific therapy. The only things you can do are: wait for the spontaneous resolution of the infection and relieve, with some effective remedies, the most annoying symptoms.
Vaccination is the fundamental preventive measure.
What is rubella?
Rubella is a contagious infectious disease, viral in origin, which causes, among the various symptoms, the appearance of small red spots all over the body.
Like chicken pox, whooping cough, mumps and measles, it is an infection typical of childhood and affects only humans.
Rubella has spread throughout the world, but since vaccination has existed, it has become a little less common.
WHO HITS?
All unvaccinated people and all those who have never had the virus in their life are at risk of rubella. Getting sick, in fact, of rubella, as well as of measles, chickenpox etc., guarantees an almost final immunity, which makes a second infection almost impossible.
Epidemiology
Rubella is considered a typically infantile infectious disease because it mainly affects children aged 1-4 and is rare among adolescents and adults.
Today, its spread, in the countries where the vaccine has been available for a long time, has dropped a lot: except, in fact, some sporadic epidemics (as in Romania and Russia between 2002 and 2004), cases per year, in many places in the world are very few.
Rubella is not a serious infection, however, if it occurs in adulthood, it is more likely to give rise to complications. In particular, in pregnant women, it can affect pregnancy and endanger the life of the fetus ( congenital rubella syndrome or CRS ).
Causes
The virus that causes rubella (also known as rubella virus ) belongs to the genus rubivirus .
Rubiviruses are part of the togavirus family (or togaviridae ), which have an outer lipid envelope, a capsid and, for genetic material, a single strand of RNA .
HOW IS THE ROSOLIA VIRUS TRANSMITTED?
By coughing, sneezing and speaking, people expel millions of small volatile droplets.
The volatile droplets coming from people with rubella contain the virus; therefore, their inhalation, by those nearby, involves the transmission of the infection.
Once inhaled, in fact, the rubella nestles at the level of the mouth and the lungs and, here, it multiplies until it reaches a numerical quota such that it can spread throughout the rest of the organism.
The transmission of the virus through volatile droplets represents a direct mode of infection.
The indirect transmission of rubella
Volatile droplets containing the virus can settle on objects and make them a means of infection. In fact, whoever touches such objects can become infected, especially if he puts his hands in his mouth or brings them close to his nose.
The transmission of the rubella that occurs with the aforementioned methods is an indirect transmission.
The viral particles survive on the surface of objects for only a few hours, after which they die.
Table . Summary of virus transmission methods.
Mode of transmission of rubella
direct:
- Volatile droplets expelled with sneezing, coughing, breathing (rare) and talking
indirect:
- Touch the objects contaminated by volatile droplets
WHEN DOES IT START AND WHEN DOES THE POSSIBILITY OF CONTAGUE STOP?
A patient with rubella is contagious since there are 7 days to the onset of symptoms 4 days after the disappearance of the rash.
Therefore, the contagiousness begins before the disease manifests itself and ends shortly after the spots on the skin are dissolved.
Symptoms
To learn more: Rubella symptoms
The symptoms of rubella appear after an incubation period of about 2-3 weeks (NB: the incubation period is the period of time that goes from the moment of infection to the appearance of the first symptoms).
The classic expressions of infection are: the skin rash (that is, the appearance of small red spots on the skin), the enlargement of the lymph nodes and a symptomatology that reminds of a cold or flu.
RASH CUTANEOUS OR SKIN ERUPTION
The skin rash, or rash or rash, is the manifestation with which rubella is usually identified.
It consists of the appearance of numerous red dots (spots).
In general, the first points involved are the ears, the head and the neck; in fact, the trunk, the legs and the arms are only involved at a later time.
For his disappearance, 3-5 days are required, not more.
LYMPHONODE OBSERVATION
The lymph nodes are small organs, belonging to the lymphatic system, which provide to defend the body from infections and threats from the external environment. In fact, they contain a discrete number of leukocytes, which are the white blood cells responsible for fighting bacteria, viruses and any other pathogenic agent.
In rubella patients, swollen lymph nodes are a fairly common expression of the disease. Their enlargement, often accompanied by pain, begins before the appearance of the skin rash and ends several weeks after recovery.
The lymph nodes usually most affected are the lymph nodes located behind the ears, those of the occipital region (ie posterior) of the head and those on the neck.
OTHER SYMPTOMS
In addition to skin rash and swollen lymph nodes, rubella can determine:
- Medium / high fever
- Typical symptoms of a cold or flu, such as a runny nose, a teary eye, a sore throat and a cough
- Reddened eyes and conjunctivitis
- Joint pain and malaise
- Loss of appetite
- Fatigue
These manifestations generally appear shortly before the rash and last for a few days.
WHEN TO REFER TO THE DOCTOR?
The enlargement of the lymph nodes located in the areas mentioned, fever and, above all, the rash are all signs attributable to rubella and to be communicated immediately to your doctor.
Attention: to contain the spread of the virus and avoid the contagion of people at risk of complications (for example pregnant women), it would be better if the first contact with the treating doctor took place by telephone.
Rubella: an infection to be reported to the competent authorities
In many countries of the world, including Italy, doctors must notify the competent health authorities of every case of rubella, even if it is a simple suspect. This measure was adopted to prevent epidemics and minimize infection.
ASINTOMATIC ROSOLIA
In some cases (according to some sources, even more than 20% of the cases), the rubella can also be asymptomatic, or not to cause, to the detriment of the affected individual, any obvious symptom.
From the immune point of view, there is no difference: in fact, asymptomatic rubella patients acquire, at the end of the infection, the same immunity of "classic" rubella patients.
Complications
Rubella is more likely to give rise to complications, if it affects individuals of adult age, pregnant women and subjects with a weak immune system (ie immunosuppressed).
In adults and in immunosuppressed subjects, the greatest danger is represented by brain infections ( encephalitis ); in pregnant women, on the other hand, the most serious danger is represented by a serious pathology, which affects the fetus and is called congenital rubella syndrome (or CRS ).
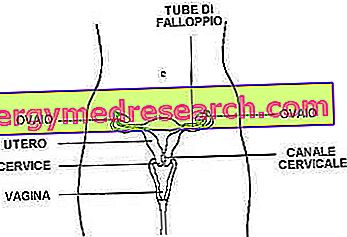
ROSOLIA CONGENITA SYNDROME (CRS)
Rubella, in pregnant women, can determine either a miscarriage ( death in utero ) or an incorrect fetal development . This second serious complication is also known as congenital rubella syndrome (CRS).
The consequences of CRS depend on the week of gestation: in fact, before the infection takes place against the mother, the effects on the fetus are more serious.
In light of this,
- If the infection occurs during the first 10 weeks, the risk of CRS is high (90%) and the effects on the baby can also be very serious.
- If the infection occurs between the 11th and 16th week, the CRS concerns 10-20% of the infected pregnant women and the effects on the child are of medium severity.
- If the infection occurs between the 17th and 20th week, the risk of CRS is very low and the effects on the child are small and of limited magnitude.
- If the infection occurs after the 20th week, it makes no sense to talk about CRS, as the infection has no repercussions on the fetus.
The CRS causes immediate effects, but also of late effects, which materialize after several years.
At the moment, unfortunately, there are no effective treatments to treat rubella in pregnant women.
The immediate and late effects of congenital rubella syndrome (or CRS)
The immediate effects of CRS on the fetus are: cataracts and other ocular deficits, deafness, congenital heart defects, a small head compared to the rest of the body (due to poor brain development), intrauterine development slower than normal, brain damage, liver damage, lung damage and, eventually, bone marrow damage.
The late effects, instead, are: type 1 diabetes, thyroid problems (hypothyroidism or hyperthyroidism) and, finally, cerebral edema (which is at the origin of numerous motor and mental disorders).
Diagnosis
To diagnose rubella, a thorough physical examination is usually sufficient, through which the whole symptomatology manifested by the patient is analyzed.
If, at the end of the physical examination, doubts still remain, it is possible to resort to two diagnostic tests with unequivocal results: the examination of the saliva, which is collected with a particular absorbent pad, or the blood tests, which is extracted from a vein in the arm.
As for the diagnosis in pregnancy, it should be pointed out that blood tests are fundamental and represent an obligatory step, given what the serious consequences of congenital rubella syndrome are.
NB: doubts about a rubella diagnosis are related to the similarity of this infection to measles or other viral infections with similar symptoms.
For further information: Rubeo Test - Blood Analysis for Rubella »
EXAMINATION OF THE SALIVA AND EXAMINATION OF THE BLOOD
In the saliva and blood of a person with rubella (or rubella in the past), there are proteins in the immune system, formed right after the viral infection. These proteins are called antibodies or immunoglobulins and serve to defend the body from infectious agents and other threats from the external environment.
Antibodies present in a person with rubella are classified as IgM ; antibodies, however, present in a person with a rubella (or vaccinated) past are classified as IgG .
DIAGNOSIS IN PREGNANCY
Given the effects of rubella in pregnancy, it is good that women wishing to have a child book blood tests so that they know whether they are protected from infection or not.
The same blood tests are recommended if a pregnant woman has come into contact with a person suffering from rubella and has been exposed to the virus.
When a pregnant woman, susceptible to rubella (ie not vaccinated or non-immune), should she contact her doctor for a blood test?
- When he had a face-to-face contact with a rubella patient
- When he spent at least 15 minutes in the same room with an individual with rubella
- When it has all the symptoms of rubella
DIAGNOSIS OF CRS
If there are grounds for suspecting congenital rubella syndrome, the diagnostic tests to which a pregnant woman (and the fetus) must undergo are an ultrasound and an amniocentesis .
Treatment
To learn more: Medicines for the treatment of Rubella
Currently there is still no drug therapy (or other) for the specific treatment of rubella.
The only things an infected person can do are:
- Wait for the spontaneous resolution of the infection (about 10 days) e
- Relieve symptoms with some special remedies / treatments
SPONTANEOUS RESOLUTION
Spontaneous resolution of rubella takes up to 10 days. In fact, so much time is needed by the immune system of a healthy person (therefore not immunosuppressed) to counteract and eliminate all traces of the virus from the body.
What happens, after healing, within the organism?
The immune system is the defensive system against threats from the external environment (first of all, viral, bacterial and parasitic infectious agents).
When it fights infectious agents such as viruses, it also prepares special defense cells, capable of recognizing the same threat in advance and preventing a second infection.
This prodigious mechanism is called immune memory and the cells that put it into practice (which are particular antibodies) are called memory cells .
Antiviral vaccines are made on the concept of immune memory.
SYMPTOMS CARE
When the infection is particularly annoying, it is possible to alleviate the symptoms with some simple remedies, sometimes very effective.
To relieve fever, generalized pain and a sense of discomfort : in these situations, it is good practice to take some anti-inflammatory and analgesic drugs, such as paracetamol and ibuprofen (which is a NSAID, which is a non-steroidal anti-inflammatory drug ).
Warning: the use of aspirin, in individuals under the age of 16, can lead to very serious side effects, such as Reye's syndrome ; therefore, it should not be administered until a certain age.
To avoid dehydration : high fever causes intense sweating, therefore, to avoid excessive dehydration of body tissues, it is necessary to rehydrate properly, so drink plenty of water.
To alleviate the effects of conjunctivitis and reddened eyes : it is essential to keep the eyes clean with special cotton buds and avoid touching them with dirty hands.
To treat cold symptoms (runny nose, cough etc.) : the main remedies for these disorders are steam inhalations and hot drinks made from lemon or honey.

Figure: steam inhalation to mitigate cold symptoms. They need a basin filled with hot water and a towel to put on the head.
For steam inhalations, it is sufficient to breathe the fumes rising from a basin of hot water and cover one's head with a towel.
To limit the spread of infection : to avoid the transmission of the disease (especially among people potentially at risk of complications, such as pregnant women) it is good practice to stay isolated at home until 4 days have elapsed since the disappearance of the skin rash . In fact, this is the minimum time required for the infectious charge (or the ability to infect other people) to run out.
Vaccination
Rubella is preventable with the MMR vaccine (where M stands for measles, P for mumps and R for Rubella) or MPRV (where M stands for measles, P for mumps, R for varicella).
This vaccination is traditionally carried out during childhood, with two injections: one at about 12-13 months and another at 5-6 years (usually shortly before starting elementary school).
What changes since 2017
With the decree law on the prevention of vaccination for minors from zero to 16 years, approved on 07/28/2017 , vaccination against rubella has become mandatory .
This specific vaccination can be performed with a single injection together with 3 other vaccination covers (the so-called quadrivalent MPRV vaccination, which includes vaccines: anti-measles, anti-rubella, anti-mumps, anti-varicella).
- The obligation of vaccination against rubella is in force, in the context of the 10 mandatory vaccinations, for those born from 2017. Even those born after 2001 are subject to the obligation of vaccination against rubella .
- Immunized subjects due to the natural disease are exempt from the vaccination requirement, therefore children who have already contracted rubella will not have to be vaccinated against this disease
Please note that compulsory vaccinations are a requirement for admission to nursery schools and kindergartens (for children from 0 to 6 years) and that the violation of the vaccination requirement implies the application of significant financial penalties .
For more information on mandatory vaccines in children, see this article.
Special case: for non-vaccinated adult individuals and children under one year of age, the vaccine is not essential / expected. It becomes, however, if the risk of a contagion is concrete. Two classic situations that require an extraordinary vaccination, so to speak, are: a trip to geographical areas where the rubella virus is highly diffused or the infection happens to a very narrow member of the family.
VACCINATION FOR CHILDREN UNDER 6 MONTHS
Children under 6 months of age and with a vaccinated or immune mother have immunity of maternal origin, which temporarily protects them; therefore, they do not need to be vaccinated.
On the contrary, children of the same age, who, however, do not have a vaccinated or immune mother, are unprotected and more prone to contract the disease. For these subjects, therefore, an injection of protective immunoglobulins could be useful.
NB: an extra injection of immunoglobulins (or antibodies), as in the aforementioned case, does not amount to a vaccine, but it can still represent a valid anti-infective solution.
VACCINATION AND PREGNANCY
To prevent the onset of congenital rubella syndrome, it is good practice for women who want a child and are not protected from infection to get vaccinated before pregnancy . The vaccine takes about a month to create the appropriate protection, so waiting times are not long.
Women who, for particular reasons, have not adopted this precautionary measure must pay close attention, because they are exposed to serious dangers. It is true that rubella is, by now, not very common, but the risk of unpleasant consequences (due to a possible infection) is concrete.
Warning: in Italy, since 2003, a national plan has been developed to eliminate congenital rubella syndrome. This plan includes, in addition to the mandatory notification of the syndrome and rubella in pregnancy, a promotion of the vaccine among people who have not yet been vaccinated.
HOW TO AVOID THE DIFFUSION OF THE VIRUS?
To avoid the spread of rubella in the best way, it is advisable for the patient to remain at home from school or work and avoid contact with people potentially at risk of complications.
The infective charge (ie the ability to infect other people) is exhausted 4 days after the disappearance of the skin rash. Therefore, it is advisable to resume normal daily activities only from this moment onwards.
WHY IS IT GOOD TO BECOME?
A large number of people vaccinated against a given virus also protect unvaccinated people, as the infection is severely hindered. This is the precious advantage offered by vaccinations that have been practiced for years, such as vaccinations for rubella, measles and mumps.