Generality
The fracture of the humerus is the rupture of the arm bone.
In most cases, episodes of fracture of the humerus are the consequence of physical trauma, accidental falls, excessive stress on the arm or the presence of particular basic illnesses.
The typical symptoms are: pain, hematoma, swelling and difficulty in moving the arm.
For a correct diagnosis, physical examination, anamnesis and X-rays are almost always sufficient.
Treatment depends on the location and severity of the fracture.
Brief anatomical revision of the humerus
In the human being, the humerus is the even bone that makes up the skeleton of the arm ; the arm is the anatomical portion of the upper limb, which runs from the shoulder to the elbow.
The humerus belongs to the category of long bones and takes part in the formation of two important joints: the glenohumeral joint of the shoulder and the elbow joint.
Like all long bones, the humerus can be divided into three main portions: the so-called proximal end (or proximal epiphysis), the so-called body (or diaphysis) and the so-called distal end (or distal epiphysis).
- The proximal end of the humerus is the portion that forms part of the glenohumeral joint and that precedes the shoulder;
- The body is the central portion of the humerus, lying between the proximal end and the distal end;
- The distal end of the humerus is the bone portion that forms part of the elbow joint and precedes the forearm.
Functionally, the humerus is important because:
- It takes part in joints fundamental for the movements of the entire upper limb, in particular arm;
- It receives the muscles that support the movements of the aforementioned joints;
- In young children, it is a support for four-legged locomotion.

What is the fracture of the humerus?
The fracture of the humerus is the skeletal injury which consists in the breaking of the bone present in the anatomical region of the human body identified with the term arm .
The most typical classification of the fractures of the humerus distinguishes the latter according to the location of the breaking point and provides for three grades: the fractures of the proximal end of the humerus, the fractures of the body (or diaphysis) of the humerus and the fractures of the distal end of the humerus.
In anatomy, proximal and distal are two terms with the opposite meaning.
Proximal means "closer to the center of the body" or "closer to the point of origin". Referring to the femur, for example, it indicates the portion of this bone closest to the trunk.
Distal, on the other hand, means "farther from the center of the body" or "farther from the point of origin". Referred (always to the femur), for example, it indicates the portion of this bone furthest from the trunk (and closer to the knee joint).
FRACTURES OF THE PROXIMAL END OF THE HUMER
At the proximal end of the humerus, there are at least 6 regions of a certain anatomical relevance: the head, the anatomical neck, the greater tubercle, the lesser tubercle, the intertubercular groove and the surgical neck.
The episodes of fracture of the humerus with involvement of the proximal extremity generally concern one of: the greater tubercle, the lesser tubercle, the surgical neck and the anatomical neck.
As regards their epidemiology, fractures of the proximal end of the humerus represent, in the general adult population, 4-5% of all cases of bone fracture.
FRACTURES OF THE BODY OF THE HUMAN
A fracture of the humerus with body involvement may be:
- A transverse fracture. The peculiarity of this injury is that the fracture gap is placed at right angles to the longitudinal axis of the bone ("horizontal" fracture).
- A spiroid fracture. The peculiarity of this injury is that the fracture line takes a spiral course along the fractured bone.
- A butterfly fracture. It is a cross between transverse fractures and spiroid fractures.
- A pathological fracture. Pathological fractures are fractures that result from concomitant pathologies that weaken the bones. Among the pathologies capable of giving rise to a pathological fracture are malignant bone tumors, benign bone tumors, metabolic diseases (eg Paget's disease), bone infections and osteoporosis.
As regards their epidemiology, fractures of the humerus body represent, in the general adult population, 3% of all cases of bone fracture.
* NB: readers interested in learning more about bone tumors can click here.
FRACTURES OF THE DISTAL END OF THE HUMER
Proceeding from top to bottom, the anatomically relevant regions of the distal end of the humerus are: the medial supracondylar ridge, the lateral supracondylar ridge, the medial epicondyle, the lateral epicondyle, the coronoid fossa, the radial fossa, the olecranon fossa, troclea and capitulum .
In most cases, fractures of the distal end of the humerus localize at the level of the supracondyloid ridges.
Regarding their epidemiology, they represent, in the general adult population, 2% of all cases of bone fracture.
Causes
The main causes of fracture of the humerus include:
- Physical traumas, resulting for example from the practice of some contact sports such as rugby, American football, football etc;
- Accidental falls or stumbling, which may occur, for example, during work or a domestic activity;
- Excessive and repeated physical stress on the arm . In these situations, doctors talk about stress fractures;
- The presence of some particular medical conditions, including osteoporosis or vitamin B deficiency . Medical conditions such as osteoporosis or vitamin B deficiency are in fact considered risk factors for humerus fractures.
CAUSES OF FRACTURE OF THE PROXIMAL END
In most cases, fractures of the proximal end of the humerus result from accidental falls, in which the victim had his arm fully extended forward. More rarely, they are the result of sports injuries or road accidents.
The main risk factors for fractures of the proximal extremity of the humerus include advanced age, the presence of osteoporosis or osteopenia and cigarette smoking.
CAUSES OF FRACTURE OF THE BODY
Among the most common causes of fracture of the humerus body are accidental falls - just like fractures of the proximal end - and physical traumas.
Among the less common causes, the metastases that originate from a breast tumor and the assiduous repetition of the gesture performed, usually by baseball players when throwing the ball, deserve a mention.
CAUSES OF FRACTURE OF THE DISTAL END
In general, fractures of the distal end of the humerus are the consequence of strong physical injuries to the elbow. In such circumstances, the olecranon of the ulna "slides" violently upwards, precisely against the distal epiphysis of the humerus.
Symptoms, signs and complications
The typical symptoms and signs of a fracture of the humerus are:
- Arm pain;
- Difficulty moving the arm;
- Swelling of the arm;
- Hematoma on the arm of variable size;
- Presence of abnormal sounds, similar to crackles, during the movements of the affected arm.
If the cause of the fracture has also impaired the good health of the nerves passing through the arm (eg radial nerve, axillary nerve etc.), there is a loss of skin sensitivity and / or muscle control, in a part of the upper limb .
If the triggering factor of the fracture has also caused an injury to the blood vessels of the arm (eg brachial artery), the patient is the victim of a reduced blood supply to the forearm and especially to the wrist.
Finally, if the fracture is broken down, the arm has a more or less accentuated deformity and the individual victim of the accident has serious difficulties to bend the elbow.
CHARACTERISTICS OF PAIN AND HEMATOMA
The pain resulting from a fracture of the humerus is immediate, in the sense that it appears immediately after the injury.
The painful sensation is so intense that the victim of the accident struggles to make even the slightest movement with the affected arm.
As far as the hematoma is concerned, however, this characteristic sign can be observed only after 24-48 hours from the accident. The size of a hematoma resulting from a fracture of the humerus varies depending on the severity of the aforementioned injury.
GRADE OF GRAVITY OF A HUMER FRACTURE
A bone fracture can be composed or decomposed, stable or unstable, simple or multi-segmental, closed or open, etc.
In general, the less serious fractures of the humerus are those compounded, stable, simple and closed, while the most serious fractures of the humerus are those which are decomposed, unstable, multi-fragmentary and open.
Readers interested in knowing the meanings of compound or broken fracture, stable or unstable fracture can click here.
COMPLICATIONS
Among the possible complications of a fracture of the humerus, fall
- Avascular necrosis (or osteonecrosis) of the head of the humerus;
- Axillary nerve injury;
- Dislocation of the glenohumeral joint;
- An injury to the rotator cuff.
Diagnosis
In general, the diagnostic procedure to which patients with a suspected fracture of the humerus are subjected includes: an accurate physical examination, a careful medical history and a series of diagnostic imaging tests.
Diagnostic imaging tests are essential to confirm any suspicion related to the presence of a bone fracture.
OBJECTIVE AND ANAMNESIS EXAMINATION
The physical examination is the set of diagnostic "maneuvers", performed by the doctor, to verify the presence or absence, in the patient, of the signs indicative of an abnormal condition.
In case of suspected fracture of the humerus, the most classic of objective examinations has as its object the painful arm and involves at least two diagnostic "maneuvers": the search for some hematoma, swelling or deformity and an assessment of the ability to move.
Moving on to the anamnesis, the latter is the critical collection and study of symptoms and facts of medical interest, reported by the patient or his family members (NB: family members are involved, above all, when the patient is small).
In case of suspected fracture of the humerus, the most classic of the anamnesis is able to reveal the possible triggering factors and the conditions of risk.
DIAGNOSTICS FOR IMAGES
The diagnostic imaging tests ideal for detecting a fracture of the humerus are:
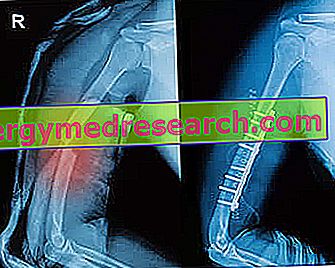
- X-rays: it is a practical examination, which clearly shows, on a photographic plate, the characteristics of a bone fracture. For example, thanks to X-rays, doctors are able to understand if a fracture of the humerus is composed, decomposed, stable, unstable, open, etc.
Although painless, it is to be considered minimally invasive, as its execution involves exposing the patient to a small dose of ionizing radiation harmful to humans.
- CT scan: is a test that provides three-dimensional images of internal organs, including bones. The images are very clear and have details that X-rays cannot grasp.
For example, unlike X-rays, a CT scan can detect any involvement of nerves in the arm or blood vessels.
The doctors use the TAC only if strictly necessary, as the exam in question, although completely painless, involves exposing the patient to a non-negligible dose of ionizing radiation harmful to humans.
- Nuclear magnetic resonance (or MRI): thanks to the creation of magnetic fields, an MRI provides detailed images of soft tissues (ligaments, etc.) and hard tissues (bones), located in the anatomical region under investigation. Completely painless, it is also a completely non-invasive test, as the magnetic fields, which are used to create images, are not at all harmful to human health.
Therapy
The treatment of a fracture of the humerus depends on the position and severity of the fracture.
In general, the rule is valid that, if the skeletal injury is not severe (ie compound fracture, stable, simple and / or closed), rest and immobilization of the affected upper limb are sufficient for at least 6-8 weeks ; while, if the injury is severe (therefore a displaced, unstable, pluriframmentary and / or open fracture), surgery is essential.
THERAPY IN THE CASE OF FRACTURE OF THE PROXIMAL END
A non-serious fracture of the proximal end of the humerus involves a conservative treatment, consisting of a period of rest, immobilization of the affected upper limb, plastering, and administration of painkillers . Generally, in these circumstances, plastering affects the arm-shoulder complex, so that it is impossible to move the upper limb, and has a duration of about 6 weeks (minimum time necessary for the joining of bone fragments).
A severe fracture of the proximal end, on the other hand, requires the intervention of the surgeon, who must first reposition the bone fragments in their correct anatomical position, and then weld them together using screws, pins, etc. At the end of surgery, rest, immobilization of the arm-shoulder complex and administration of painkillers, against pain, are a must. Usually, rest and immobilization should last between 6 and 8 weeks.
THERAPY IN CASE OF BODY FRACTURE
Most fractures of the humerus body are such that conservative treatment is sufficient. As in the previous case, conservative treatment is based on: rest, immobilization of the arm-shoulder complex and administration of painkillers.
The use of surgery is rare and is usually expected when the fracture is associated with damage to blood vessels or nerves in the arm.
Generally, rest and immobilization - whether the treatment has been preserved or surgical - should last between 6 and 8 weeks.
THERAPY IN CASE OF FRACTURE OF THE DISTAL END
In general, the treatment of fractures of the distal end of the humerus is conservative and consists of: rest, immobilization of the arm-elbow complex and administration of painkillers.
The surgeon's intervention is expected only in the presence of damage to the nervous and / or vascular structures, or in the presence of displaced, unstable, open fractures etc.
Rest and immobilization must last until the reunion of bone fragments, which generally takes between 6 and 8 weeks.
HOW TO UNDERSTAND IF YOU HAVE HAD THE HEALING?
Whether in the presence of severe fractures, or in the presence of non-serious fractures, the only way to ascertain the welding of the humerus is to observe its state of health, by means of an X-ray examination.
If, based on the X-ray examination, some bone lesion persists, the treating physician is forced to immobilize the arm-shoulder or arm-elbow complex again and to recommend more rest.
PHYSIOTHERAPY: A FUNDAMENTAL STEP
Any fracture of the humerus requires, after the period of rest and immobilization of the upper limb, a cycle of physiotherapy sessions.
In such circumstances, physiotherapy is used to restore joint mobility of the shoulder and elbow, to strengthen the upper limb muscles immobilized for a long time, etc.
The ultimate goal of physiotherapy is to restore the normal function of the entire upper limb, which has suffered the fracture of the humerus.
Prognosis
The prognosis of a properly cured humerus fracture depends on the severity of the fracture. This means that less severe fractures have a better prognosis than more serious fractures.
Final healing from a fracture of the humerus can take between 4 and 10 months.



