Generality
Glomerulonephritis is an inflammatory disease that affects the kidneys, particularly the renal glomeruli, compromising its filtering capacity. Because of the inflammatory process that affects the kidneys, the meshes of the renal sieves widen, and the glomeruli let out normally retained blood components: this is the case of proteins and red blood cells, which in the presence of glomerulonephritis are found in excessive quantities in urine.
This loss depletes the blood of important components for the balance of body fluids, with the possible appearance of edema, anemia and hypertension.
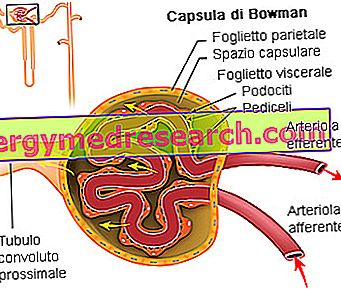
Depiction of a renal corpuscle: it is formed by a vascular portion (consisting of a ball of arterial capillaries called the renal glomerulus) enclosed by an epithelial capsule (Bowman's capsule).
The latter is composed of two epithelial sheets: the parietal and visceral leaflet; the latter is composed of particular cells called podocytes.
A chamber called the glomerural chamber is created between the two epithelial sheets, inside which the renal filtrate is poured
The podocytes have extensions (the pedicels), with which they reach the capillary epithelium. These cells are negatively charged and have small gaps that prevent the passage of larger molecules present in the blood. When damaged by an inflammatory process, the podocytes increase their permeability, allowing large molecules such as proteins to pass.
The inflammatory process associated with glomerulonephritis is generally symmetrical and bilateral, so it involves the glomeruli of both kidneys.
There are numerous forms of glomerulonephritis, with different pathogenesis, course and prognosis, ranging from asymptomatic forms to lethal evolving forms in an acute or chronic way towards renal failure. The element that acts as a glue between the various forms is the presence of an inflammatory damage of the renal glomeruli, for the rest there is a wide variability both for the causes of origin and for the most appropriate treatment.
First of all, acute and chronic forms and primitive and secondary forms are distinguished.
- Acute glomerulonephritis: sudden onset of hematuria and proteinuria, accompanied by rapidly progressive renal failure, with edema, hypertension, and increased serum creatinine and azotemia
- Chronic glomerulonephritis: reduction of slow and progressive renal function, with urinary finding of hematuria and proteinuria, which slowly leads to the uremic syndrome; the onset of renal failure takes days or years and is the consequence of wear damage of the surviving nephrons due to functional compensatory overload. Proteinuria, generally present, does not exceed 3 g in 24 hours
- Primary glomerulonephritis: affects only or mainly the kidney: the problem, the responsible cause of the disorder, therefore lies at renal level
- Secondary glomerulonephritis: is the expression of pathologies affecting other organs or the entire organism (systemic diseases such as systemic lupus erythematosus or diabetes)
Sometimes the glomerulonephritis cannot be traced back to a precise cause, since doctors cannot identify the causative etiopathological element: in this case, we speak of idiopathic glomerulonephritis.
Renal glomerulus and kidney functions
The nephron is the functional unit of the kidney, that is, the smallest anatomical formation capable of performing all the functions for which the organ is responsible. Each of the two main nephrons around each kidney is divided into two essential components:
- renal or Malpinghi corpuscle (glomerulus + Bowman's capsule): responsible for filtration;
- tubular system: responsible for resorption and secretion;
and carries out three fundamental processes:
- filtration: it takes place in the glomerulus, a highly specialized capillary system that allows all the small molecules of the blood to pass through, opposing only the passage of larger proteins and blood cells;
- reabsorption and secretion: they occur in the tubular system, with the aim of recovering excessively filtered substances (eg glucose, which the body cannot afford to lose with urine) and to eliminate those filtered inadequately.
Symptoms and complications
See also: Nephritis symptoms
The main clinical manifestations of glomerulonephritis are hematuria, proteinuria, impaired renal function, arterial hypertension, edema.
On the clinical level, it is important to distinguish:
- Glomerulonephritis associated with nephritic syndrome: characterized by proteinuria, haematuria associated with blood cylinders, arterial hypertension, edema from sodium and water retention, normal or reduced renal function; it is caused by an increase in glomerular permeability and an inflammatory damage of the glomerular capillaries
- Glomerulonephritis associated with nephrotic syndrome: characterized by proteinuria without hematuria, hypoalbuminemia and edema, hyperlipidymia and lipiduria; it is a less severe condition than the previous one, since there is an increase in glomerular permeability with preservation of renal functions, without passage of red blood cells in the urine
Deepening: How do the symptoms of glomerulonephritis arise?
Inflammation and glomerular damage
↓
Severe permeability alterations
↓
Proteinuria = significant loss of protein with urine → foam may be seen in the urine
↓
Hypoproteinemia (or hypoprotidemia or hypoalbuminemia) = reduction of proteins in the blood (in particular of albumin, the most abundant plasma protein)
↓
Reduction of the oncotic (or colloidosmotic) pressure of plasma + lipiduria due to hyperlipidemia caused by the stimulus on the synthesis of lipoproteins in the liver and by the urinary loss of some factors that regulate lipid metabolism
↓
Liquid displacement in the extracellular spaces → Appearance of edema (initially in the morning at periorbital level, then extended to the feet, ankles and abdomen) + Hypovolemia + Reduction of blood pressure
↓
Reduction of blood flow to the kidney
↓
Increased renin secretion → Activation of the renin-angiotensin system + Increased release of aldosterone → hydrosaline retention and exacerbation of edema + Mild hypertension → Increase in hydrostatic pressure in the glomerulus, increase in filtration process → wear of nephrons due to functional overload
Glomerular damage with rupture of the endothelial layer of the glomerular capillaries
↓
Severe permeability alterations
↓
Hematuria = presence of blood in the urine → in the case of macrohematuria the urine takes on a dark color, similar to tea or coca-cola; in the case of microhematuria, the presence of blood in the urine can be seen only by the chemical-enzymatic examination of the urine
↓
Anemia = reduction in the concentration of red blood cells and hemoglobin in the blood, may also result from the urinary loss of ferritin due to an increase in glomerular permeability (it is therefore also found in the case of glomerulonephritis associated with a nephrotic syndrome)
↓
Weakness, fatigue
The inflammatory damage to the renal glomeruli, with infiltration of white blood cells and obstruction of the capillaries, leads to a reduction in the glomerular filtration rate
↓
Increased renin release from the iuxtraglomerular apparatus with activation of the renin-angiotensin-aldosterone system
↓
Increased water and sodium retention, also due to the lower excretory capacity of the kidney (in particular sodium)
↓
Hypertension (Note: Hypertension can also be a predisposing cause of glomerulonephritis, since pushing the blood more strongly against the capillary walls of the glomerulus favors the escape of proteins and erythrocytes in the urine)
↓
Increased hydrostatic blood pressure, which together with the reduction of oncotic pressure favors the appearance of edema
Renal damage resulting from glumerolonefrite (release of proteolytic enzymes and inflammatory cytokines, formation of fibrin deposits) can also increase the presence of waste products in the circulation, due to loss of filtering capacity of the nephron → on the clinical level it can be associated with hyperazotemia and hypercreatininemia → trend towards evolution towards renal failure
Continue: Glomerulonephritis: causes and therapy »



