What is that?
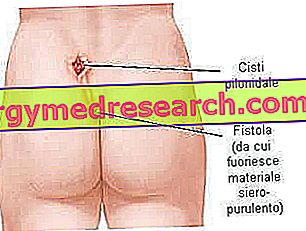
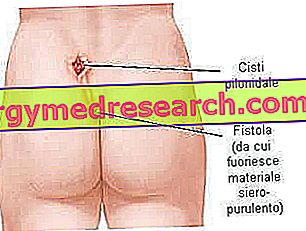
The pilonidal cyst is a saccular lesion that develops in the skin, almost always in the sacro-coccygeal region, just above the intergluteal groove.

Pilonidal cysts are harmless until they undergo infection and inflammation. If a pilonidal cyst becomes infected, it can degenerate into an abscess, which is often extremely painful. Furthermore, the pus collected in the cavity can determine the onset of a fistula.
Anyone can develop a pilonidal cyst, but the lesion is more common in young Caucasian men, aged 15 to 24 years. In particular, people who sit for long periods of time, such as truck drivers, are at greater risk of developing the injury. Treatment and management of pilonidal cysts depends on many factors, including the extent and chronicity of the disease. A complete cure is possible, but a cystic cavity can recur even if removed surgically. Recurrence of the lesion is, in fact, a common occurrence, estimated in about 40-50% of patients.
Cysts, abscess and fistula
The terms cyst, abscess and pilonidal fistula refer to three different phases of pilonidal disease:
- The pilonidal cyst is a small uninfected pouch, similar to a small nodule, asymptomatic or slightly painful on palpation. The lesion can remain silent for years or evolve in the later stages.
- The pilonidal abscess is a collection of pus that originates from the bacterial infection of the cystic cavity. This formation is larger than the previous one and involves pain, redness and other characteristic signs of inflammation. After a few days, the abscess undergoes breakage and fistula with immediate improvement of the conditions. However, if it is not adequately treated, the inflammatory process does not stop spontaneously and tends to become chronic.
- A pilonidal fistula is a small opening (or communication channel) between the infected cyst and a cutaneous orifice that provides an outlet to the outside:
Symptoms
A pilonidal cyst is a lesion that develops centrally in the lower back, at the level of the coccyx, near the fissure of the buttocks, at about 4 -5 cm centimeters from the anus. Some individuals may remain asymptomatic for some time before the acute inflammatory process is presented. Symptomatic disease usually occurs when the pilonidal cyst degenerates into a pilonidal abscess: the patient feels greater discomfort, the local swelling is more noticeable and the area is painful to the touch.
If the pilonidal cyst becomes infected, the following signs and symptoms may develop:
- Signs of abscess inflammation: pain, swelling, redness and heat of the affected skin region;
- Secretion of purulent (or serum-purulent) material, yellowish and smelly;
- Fever (uncommon), headache and general malaise.
These symptoms can develop quickly, often in a few days. The pain caused by a pilonidal fistula can be severe and is likely to worsen if treatment is not used.
Less commonly, the pilonidal cyst can develop in other areas of the body, such as the hands, the navel, the axilla or the genital region.
Causes
Although there are several theories on the causes of pilonidal disease, today most researchers believe that cysts are acquired lesions (rather than congenital or innate as believed in the past); their onset would be related to an infection of the hair follicle which, once dilated, would allow the hair to be encased. In response to these ingrown hairs, a local inflammatory reaction develops which causes the formation of a cystic structure.
Excessive pressure, friction or repeated trauma in the sacro-coccygeal region may predispose individuals to develop cysts or cause irritation to an existing pilonidal lesion.
Risk factors
Some factors may predispose to the development of the pilonidal cyst. These include:
- Obesity: obese individuals are more likely to have relapses;
- Sports or occupational activities that require a prolonged sitting position (increases the pressure on the coccyx region);
- Poor hygiene and the presence of many unwanted hairs;
- Excessive sweating: humidity favors the growth of anaerobic bacteria, which often infect the pilonidal cysts;
- Local irritation or trauma, which can cause inflammation of an already existing cyst or promote its onset;
- Wear tight clothing.
Diagnosis
A pilonidal cyst can be diagnosed by a simple clinical examination, based on the characteristic signs in the coccygeal area: presence of external orifices, secretion of liquid or purulent material, etc. The area is extremely painful on palpation and, often, the simple act of separating the buttocks to examine the area is intolerable for the patient. To define the diagnosis it may be useful to also use blood tests and a targeted ultrasound.
The doctor can also detect the presence of the following conditions:
- Temperature;
- Increased white blood cells on a blood sample;
- Inflammation of the surrounding skin.
Possible complications
Complications of a pilonidal cyst may include:
- Recurrence of the pilonidal cyst;
- Abscess formation and chronic suppuration;
- Systemic infections;
- Rarely, if the chronic pilonidal cyst is not treated properly it can degenerate into a squamous cell skin carcinoma.
surgical
Pilonidal cyst therapy is surgical.
Patients who do not have local inflammation generally do not require any immediate treatment, but are advised to hair removal and meticulous local hygiene. If instead an infection develops at the level of the cystic cavity it is necessary to resort to an adequate treatment to drain or remove the lesion.
Incision and drainage of the pilonidal cyst
The first therapeutic approach involves a surgical procedure that can be performed on an outpatient basis.
- After numbing the area with a local anesthetic, the doctor makes a small incision over the infected area to open the cystic cavity.
- The purulent material is drained, all hair and other fragments accumulated in the cyst are removed. The wound is cleaned with saline solution and covered with sterile gauze.
- Dressings must be replaced frequently, until the cyst is healed (approximately three times a week).
- Your doctor may prescribe some antibiotics, such as metronidazole and erythromycin, to treat inflammation and avoid bacterial reinfection. Often, painkillers are prescribed for symptomatic treatment.
A medical check-up should be organized in the two days following the procedure, to assess whether the wound is healed properly and to monitor for any complications. Once the dressings are removed, the skin wound heals and closes spontaneously in about four weeks. Most people subjected to incision and drainage of the pilonidal cyst do not need any other treatment. Keeping the wound clean and removing all the hairs in the sacro-coccygeal area can help prevent recurrences.
Excision of the pilonidal cyst
If you have a pilonidal cyst that tends to get infected in a recurrent way, you may need a more invasive surgery to remove all the tissue affected by the cyst (skin, subcutaneous tissues and cystic area up to the sacrum). Excision allows the condition to be completely cured but is a rather invasive procedure compared to simple incision and drainage.
After excision of the pilonidal cyst, the doctor may choose to:
- Leave the surgical wound open (closing by second intention). In this option, the surgical wound is left open, without proceeding to any suture, so as to allow the tissue to spontaneously reform itself from the base towards the surface. This process results in a longer healing time, but is associated with a lower risk of recurrence (recurrent infection of the pilonidal cyst). Sometimes, a simple sterile gauze swab is inserted into the surgical wound. Healing takes place in a time varying between 5 and 8 weeks, during which the dressings must be changed by expert personnel, on average every three days.
- Close the wound with stitches (closure by first intention). After removing the pilonidal cyst, some surgeons prefer instead to immediately close the wound with stitches. The healing time is faster with this option, but is associated with a greater risk of relapse. Some surgeons perform the incision at the level of the intergluteal groove, an area where healing is particularly difficult. The stitches are removed after about 10-12 days. Recovery time after surgery can take several weeks.
Possible post-operative complications may include a local infection or poor healing of surgical wounds. To avoid such consequences, the doctor or nurse will provide the patient with detailed instructions regarding wound management and the course of a normal healing process. It may also be necessary to shave around the surgical site to prevent hair from entering the wound. During the post-surgical phase, outpatient care and check-ups are necessary to ensure proper wound healing and to manage the possible complications or recurrences of pilonidal disease. Although 40-50% of patients may experience recurrences of pilonidal disease, in general, the long-term prognosis is excellent.
Other less common interventions that can be performed in the case of pilonidal cysts are:
- Phenol injections;
- Skin transplants.
Prevention
To help prevent acute or recurrent pilonidal cysts, you can try to:
- Keep the area clean and dry, scrupulously taking care of local hygiene;
- Prefer the use of comfortable clothing to prevent the fabrics from rubbing against the skin;
- Keep the area free from unwanted hair by regularly using depilatory creams or laser hair removal;
- Avoid prolonged sitting position or excessive repetitive pressure for the coccyx area;
- In obese subjects, weight loss can help reduce the risk of relapses.