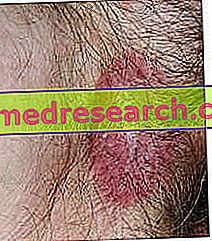
Like caries, periodontitis is also a polymicrobial infectious disease. The inflammation of the periodontium is in fact caused by different pathogenic species, which contribute to creating damage to the tissues surrounding the tooth and which ensure its mechanical stability (gingiva, periodontal ligament and alveolar bone). Over time, periodontopathies cause destructive lesions of the collagen fibers and alveolar bone, to the point of causing the tooth to fall.
Inside the mouth there are some hundreds of different microbial species; some of these are harmful, others neutral and others still can be considered beneficial (they are opposed to the proliferation of harmful species). The composition of the oral microbial flora is strongly influenced by diet, oral hygiene level and genetic factors.
Regarding the origin of periodontitis, it is necessary to focus on the microbial species present in the so-called subgingival plaque. In fact, between the free margin of the gingiva and the enamel of the tooth there is a furrow, 1-2 mm deep, called the gingival sulcus; in some ways, this groove represents a sort of ecological niche, a small pocket that offers protection against bacteria that are not very tolerant to oxygen.
If in the caries the main cariogenic microorganisms are some streptococci (in particular S. mutans ), in the periodontitis they are mostly involved anaerobic Gram-negative bacteria, represented above all by the genera Bacteroides and Fusobacterium .
To be sure, under normal conditions the subgingival plaque does not differ much from the supragingival plaque and only about 12% of the cultivable subgingival flora is made up of anaerobic and microaerophilic Gram-negative bacteria. However, if oral hygiene is insufficient, the percentage of anaerobic species tends to increase and grows more and more as the gums become inflamed (gingivitis) and the gingival sulcus deepens (a gingival sulcus rendered pathologically by the periodontal disease gets the name of gum pocket ).
The main etiological agents of periodontitis include Fusobacterium nucleatum, Prevotella intermedia, Porphyromonas gingivalis and Treponema denticola . The Entamoeba gingivalis parasite was found in 95% of people with gum disease and rarely in people with healthy gums.
The presence, even abundant, of microorganisms with a strong pathogenic potential is not sufficient to determine periodontitis. The inflammation of the supporting tissues of the tooth is in fact maintained by a chronic hyper-activation of the immune system, which on the one hand fights the invaders and on the other creates damage to the periodontal tissues. In fact, the endotoxins released by the destruction of the bacteria stimulate the activity of the osteoclasts, which release some mediators responsible for the destruction of the periodontal tissues.
Factors such as diabetes and cigarette smoking raise the risk of suffering from periodontitis because they reduce the flow of blood (and oxygen) to the gum tissues, favoring the proliferation of anerobic species. Anomalies in the shape and position of the teeth, carious cavities, fillings and malformed prostheses, unsuitable orthodontic equipment and insufficient oral hygiene raise the risk of periodontitis because they favor plaque accumulation and retention.