Related articles: Sepsis
Definition
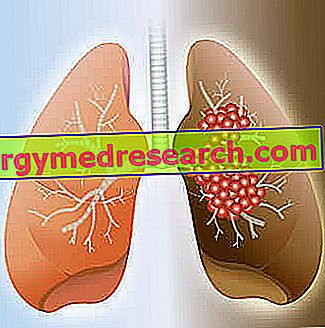
Sepsis (or septicemia) is an acute inflammation that results from excessive systemic response to a bacterial infection. It is a serious pathological condition determined by the passage of pathogens from localized infectious foci into the blood.
The most frequently involved causative agents are Gram-negative bacteria, Staphylococci, Streptococci and Meningococci. Acute pancreatitis and major trauma, including burns, can occur with signs of sepsis. Immunodepression or severe debilitation (eg diabetes, malnutrition, liver or kidney failure) can promote the development of a generalized infection.
The evolution of sepsis can be variable: some forms lead to death in a few days, others present a slow course with possible exacerbations. In addition, sepsis can progress to septic shock.
Most common symptoms and signs *
- Respiratory acidosis
- Anuria
- Chills
- Cachexia
- Bad digestion
- Cyanosis
- Coma
- Skin discoloration
- Dyspnoea
- Bruising
- Edema
- Rash
- Temperature
- Glycosuria
- Hypercapnia
- Hyperglycemia
- hyperpnea
- Hyperventilation
- Hypocalcemia
- Hypoxia
- Hypotension
- Hypothermia
- Hypovolemia
- Lethargy
- Leukopenia
- Headache
- marasma
- Fetal death
- oliguria
- Pallor
- thrombocytopenia
- Nephritic syndrome
- splenomegaly
- Confusional state
- Sweating
- Tachycardia
- tachypnoea
Further indications
In addition to the symptoms related to the infection, sepsis presents with high fever, chills and sweating, hypothermia, tachycardia, increased respiratory rate, consistent reduction of diuresis, confusion, edema and general condition impairment. Headaches, exanthematous eruptions, bruising or bleeding, increased spleen volume and infective abscesses may also occur.
Severe sepsis manifests as hypotension, oliguria, sensory changes and signs of compromise of at least one organ. Organic dysfunction produces further specific symptoms and signs: cardiovascular decompensation typically manifests itself with hypotension, respiratory failure with hypoxemia, renal failure with oliguria and haematological decompensation with coagulation dysfunction.
Early diagnosis is essential for the management of sepsis. When a patient develops signs of systemic inflammation, physical examination and diagnostic tests (including urine testing and urine culture, blood cultures and cultures of other suspected body fluids) allow you to demonstrate its presence and isolate the responsible bacterium.
Laboratory tests, in particular, show leukocytosis (white blood cell count> 12, 000 / mm3) or leukopenia (GB <4000 / mm3), reduction in the number of platelets, moderate anemia, presence of albumin in the urine, increase in protein C- reactive and plasma procalcitonin.
Within 6 hours of suspected diagnosis, a treatment based on the massive infusion of fluids, antibiotics, surgical removal of infected or necrotic tissues, pus drainage and support assistance (intubation, dialysis, etc.) must be instituted. Early therapy is essential to reduce mortality.