Generality
Patellar chondropathy is a painful condition, characterized by the deterioration and softening of the cartilage layer located on the inner side of the patella.

The typical symptoms of patellar chondropathy are pain at the kneecap and the sensation of crunching at the knee, when the patient bends the joint.
For a correct diagnosis of patellar chondropathy, physical examination, medical history and diagnostic imaging tests are useful.
The therapy includes rest, application of ice, use of anti-inflammatories and, in the most serious cases, physiotherapy and surgery.
Short anatomic recall of the patella
The patella, or patella, is the protruding bone, detectable by touch, which is located on the front of the knee joint.
Similar to an inverted triangle, the kneecap is in communication with:
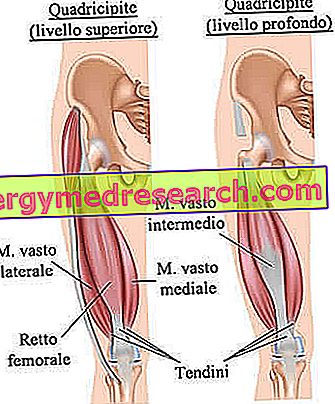
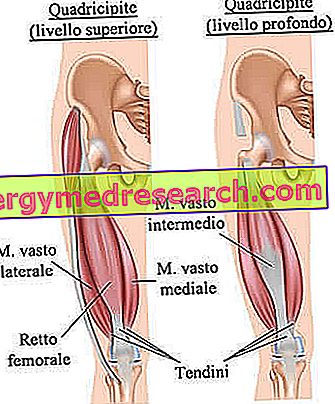
- The femur (thigh bone), by means of the tendons deriving from the muscles, which constitute the so-called quadrate (thigh muscle group);
- The tibia (leg bone), through a ligament, called the patellar or patellar ligament .

- Ensure leg extension and bending. The patella is not a static bone; for example, during the bending movement of the leg, it goes up, called up by the quadriceps tendons.
- Increase the efficiency of the quadriceps muscle.
- Protect the internal structures of the knee.
What is patellar chondropathy?
Patellar chondropathy is a painful condition, characterized by the deterioration and softening of the cartilage present on the inner side of the knee patella.
This cartilage acts as an anti-friction pad, preventing rubbing of the patellar bone with the other bones of the knee joint.
Readers are reminded that the knee is an articulation that includes three bony elements, which are the femur (to be precise, the distal portion), the tibia (proximal portion) and the patella, as well as numerous other anatomical elements, including: meniscus, ligaments, synovial bags, etc.
What is a chondropathy?
Condropatia is the non-specific term by which doctors indicate any cartilage disease, either this cartilage belonging to the hyaline type, the elastic type or the fibrous type.
In the table below, the reader can review the types of cartilage tissue present in the human body and their main location.
| Types of cartilage in the human body | Location (examples) | Features |
Hyaline cartilage | Ribs, nose, trachea, bronchi and larynx | Bluish white in color, it is the most common type of cartilage in the human body. It is not present in the joints. |
Elastic cartilage | Auricles, Eustachian tube and epiglottis | Matt yellow in color, it has remarkable elasticity. |
Fibrous cartilage | Intervertebral discs, knee menisci and pubic symphysis | Of whitish color, it is particularly resistant to mechanical stress. It is richly present in the joints. |
SYNONYMS
Patellar chondropathy is known by several other names, including: patellofemoral condropathy, patellar chondromalacia, chondromalacia patellar, femoro-patellar pain syndrome and runner's knee .
Causes
The onset of patellar chondropathy depends on improper movement of the patella, which involves rubbing its inner part against the distal portion of the femur.
In other words, the patellar chondropathy is the consequence of a repeated rubbing of the patella against the portion of the femur involved in the formation of the knee joint.
Rubbing the patella against the femur generates inflammation .
WHAT CAN UNLOAD THE ROTULA'S MOVEMENT?
Possible causes of improper patella movement are:
- Congenital malformations, which determine the absence of a correct alignment between the femur, patella and tibia.
- The presence of an anterior and posterior musculature of the thigh is very weak.
- A strong imbalance between the adductor muscles of the thigh (inner side) and the abductor muscles of the thigh (outer side).
- A strong trauma to the patella.
RISK FACTORS
According to the experts, they are risk factors of the patellar chondropathy:
- The youth age . Patellar chondropathy is more common among adolescents and young adults, as these subjects have bones and muscles that are still growing, and therefore more susceptible to abnormal behavior (such as rubbing the kneecap on the femur).
- Membership in the female sex . The greater exposure of women to the patellar chondropathy would seem due to the lower muscle mass, which characterizes the female population.
- The presence of flat feet . Those who suffer from affected feet tend to develop knee problems more easily, including the patellar chondropathy.
- The patella injuries, such as the patellar dislocation (or patellar dislocation ).
- Sports activities practiced at a high level, involving continuous knee stress and lower limbs in general.
- Arthritis in the knees . Arthritis is the medical term for any inflammatory process involving one or more joints.
Symptoms and Complications
The classic symptoms of patellar chondropathy are pain in correspondence with the kneecap - a pain that doctors define with the femoral-patellar adjective - and the strange sensation of "something that pops" at the time of the extension / bending movements of the affected knee.
PECULIARITY OF PAIN
Femoro-patellar pain tends to worsen in different situations.
The two circumstances that most commonly aggravate the painful sensation are: spend many hours standing and continuing in the practice of physical activities, which require the use of the knees and lower limbs in general.
WHEN TO REFER TO THE DOCTOR?
If a person experiences suspicious knee pains that, despite resting, tend not to heal, they should contact their doctor and request a consultation.
If the need to investigate the origin of the symptomatology with more specific assessments and tests emerges from the consultation, it would be essential to have a specialist visit to an orthopedic doctor.
Diagnosis
In general, the diagnostic procedure for the detection of patellar chondropathy starts with an accurate physical examination and a careful medical history, and ends with one or more diagnostic imaging tests.
In the event that doubts persist after these canonical investigations, the doctors could also prescribe an arthroscopy with diagnostic purposes.
OBJECTIVE AND ANAMNESIS EXAMINATION
The objective examination is the set of diagnostic maneuvers, carried out by the doctor, to verify the presence or absence, in the patient, of signs indicative of an abnormal condition.
In the presence of a suspected patellar chondropathy, diagnostic maneuvers are aimed at assessing the position and movement of the patella, with respect to the femur and tibia.
The anamnesis, instead, is the collection and the critical study of the symptoms and the facts of medical interest, reported by the patient (or his relatives).
Physical examination and medical history are two very important assessments, from which the doctor can draw many useful information.
EXAMS OF DIAGNOSTICS FOR IMAGES
In the case of patellar chondropathy, the most significant diagnostic imaging examinations are: nuclear magnetic resonance (NMR) and X-rays .
A knee MRI shows quite clearly the state of joint cartilage health (including the cartilaginous tissue of the patella).
Knee X-rays allow us to assess the condition of the bones involved in the joint; moreover, it is useful in the diagnosis of arthritis (NB: arthritis is one of the risk factors for patellar chondropathy).
DIAGNOSTIC ARTROSCOPY
An arthroscopy is a minimally invasive surgical procedure, which allows the diagnosis and treatment of various types of joint diseases.
From the procedural point of view, it consists in the introduction, in the suffering joint, of an instrument equipped with a camera and connected to an external monitor; if performed for therapeutic purposes, the arthrocentesis foresees the further introduction of surgical instruments for the correction of the joint problem.
To obtain a safe diagnosis of patellar chondropathy, arthroscopy is the most indicated test.
DEGREE OF ROUNDED DRYPROPATHY
An accurate and precise diagnostic procedure allows the doctor to quantify the severity of a patellar chondropathy.
Knowing how severe the chondromalacia patella is allows you to determine which is the most appropriate therapy.
According to experts, a patellar chondropathy can be characterized by 4 degrees of increasing gravity:
- Grade 1: means that the patellar cartilage has a slight softening. It is the least severe grade.
- Grade 2: means that the patellar cartilage has a softening and small superficial erosions.
- Grade 3: means that the patellar cartilage has thinning and significant deterioration.
- Grade 4: means that the patellar cartilage has serious erosions, so that the bone of the underlying patella is visible. It is the most severe degree.
Treatment
The goal of the treatment of patellar chondropathy is to avoid rubbing the patella on the femur, thus preventing erosion of the patellar cartilage.
For less severe cases, the therapy includes an absolute rest period from any stressful activity on the knees, the use of anti-inflammatories and the application of ice on the painful knee.
For cases of medium or severe severity and for recurrent ones, the aforementioned treatments may be added by the treating physicians: physiotherapy and arthroscopic surgery, for the appropriate replacement of the patella.
ANTI-INFLAMMATORY MEDICINES
Generally, the prescribed anti-inflammatory medicines belong to the category of NSAIDs (Non-Steroidal Anti-Inflammatory Drugs).
APPLICATION OF ICE
The application of ice on the painful joint must take place 3 to 5 times a day, for no more than 20 to twenty minutes.
Ice therapy, combined with rest, is called RICE, where R is "Rest" (in English it is " Rest ") and ICE for "ice".
PHYSIOTHERAPY
Physiotherapy consists of exercises for strengthening and lengthening the anterior (quadriceps), posterior (the so-called hamstring ), inner (adductor) and external (abductor) muscles of the thigh.
Physiotherapy exercises are particularly useful in the presence of a misalignment between the femur, patella and tibia.
THERAPEUTIC ARTHROSCOPY
Therapeutic arthroscopy is an intervention that does not require any hospitalization. The patient, in fact, can leave the hospital a few hours after the operation is completed, once the effects of local anesthesia have completely vanished.
Prognosis
Generally, patellar chondropathy has a positive prognosis.
Possible problems are more frequent in the most serious cases.
With regards to recovery times, it is important to point out that a case of grade 1 patellar chondropathy heals faster than a case of patellar chondropathy in grade 2 or higher.
Prevention
Properly protect the knees during all those activities that involve the impact of the patella on the ground / floor, maintain a certain muscular balance between the various muscles of the thigh and remedy the presence of flat feet with appropriate footwear (if you clearly suffer from this problem) are the main preventive measures, to reduce the risk of patellar chondropathy.