Introduction

Diagnosis
The diagnosis of a keloid is rather easy and consists in the simple objective examination of the lesion by the doctor.
The macroscopic characteristics of a keloid, detected by clinical diagnosis, can be summarized as:
- Initially intense red color of the lesion; subsequently, the colors fade to rosy or brownish
- Absence of hair follicles
- Scar healing not spontaneously resorbable
- Clear magnification of the initial wound and extension in the neighboring areas
- Irregular texture and rubbery consistency of the lesion
On histological examination, in a keloid a cellular infiltrate and an exaggerated accumulation of extracellular matrix (mainly composed of type III collagen and hyaluronic acid) are observed.
Sometimes, the keloid causes itching, discomfort or soreness in the area in which it arises, which is accentuated with movements or pulling the skin in the affected site. When a keloid originates near a joint, the patient may experience a reduction in limb mobility.
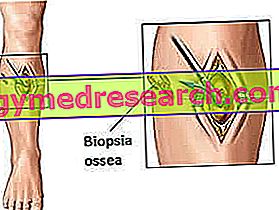
A skin biopsy may be necessary in the presence of a suspected tumor lesion (eg melanoma).
Treatment
With many probabilities, the normal surgical removal of the keloid would lead to a new lesion, thus laying the foundations for the formation of a further cicatricial process (with the formation of a thicker and extended keloidal scar compared to the previous one). To avoid similar consequences, very often the doctor offers the patient a conservative or alternative approach.
The possibilities of intervention to improve the skin affected by keloid are:
- Intralesional cortisone injections (elective therapy for the treatment of keloids): the practice, not excessively painful, is quite safe and the benefits are very good. Normally, the patient must undergo a cortisone injection a month: after several treatment cycles, the keloid is flattened and its presence is undoubtedly less conspicuous. It is estimated that 70% of patients suffering from keloids and treated with cortisone injections are satisfied with the outcome; despite this, the recurrence rate is very high.
- Laser therapy: a widely used method, the laser flattens the keloid making it, over time, less visible. Laser treatment induces progressive keloid regression by suppressing fibroblast proliferation. Although the intervention is effective, safe and not very painful, it is necessary to undergo more treatments (which are rather onerous) to obtain satisfactory results.
- Interferon injection (small group of proteins produced by the immune system in response to infections caused by pathogens such as bacteria, viruses and fungi): a method that involves injecting this substance directly into the keloid to reduce its extension and size. Being innovative, this method is surrounded by a cloud of doubts and controversies; many experts are doubtful about the long-term effectiveness of this treatment. As an alternative to interferon injections, some researchers believe that topical (local) application of immunomodulatory drugs such as imiquimod may be beneficial for keloid healing as it would stimulate the body to produce interferon.
- Fluorouracil injections: some researchers are of the opinion that the topical injection (in situ) of this chemotherapeutic agent can be used in monotherapy, or in association with corticosteroid injections and / or with the laser, to reduce the keloid extension .
- Silicone sheets (eg silicone hydrogel): despite the prolonged application (for a few weeks) of silicone sheets directly on the keloid is not a guarantee of success to remove these injuries, some experts are confident and propose this type of treatment at patient. The results are variable: generally, this approach is indicated for the management of symptoms (pruritus, discomfort) in patients with stable keloids and for the prevention of recurrences, rather than for the effective treatment of keloid.
- Cryotherapy: method that consists in the literal freezing of the keloid lesion with liquid nitrogen. The limit of this treatment is hypopigmentation (discoloration of the skin in which there is a progressive loss of tonality of the same), which makes this procedure impossible for people with dark skin.
- Radiation: some doctors propose radiation to flatten or obscure the keloid. Although the result is good, radiotherapy is not always indicated because long-term side effects (increased risk of skin cancer) far outweigh the benefits.
Prevention
The best treatment for keloid treatment is prevention: each of us should avoid unnecessary trauma or surgery (including simple ear piercings, tattoos and cosmetic surgery). Furthermore, any skin disorders - such as acne and infections - should be treated immediately, therefore starting from the appearance of the first symptoms, to minimize the inflamed areas.
To prevent a keloid already formed from degenerating and increasing in size, it is important to keep the scar always clean.
Again, to prevent the cheloid scar from magnifying and causing discomfort, we recommend daily or multi-daily application of nourishing and antioxidant creams.
To conclude, it is not possible to dictate a generic prophylactic line against keloids: the only important trick is to avoid unnecessary interventions or traumas that could degenerate into non-reversible scars such as keloids.