What is Vasculitis
Vasculitis: key points- Vasculitis is an inflammation of the blood vessels.
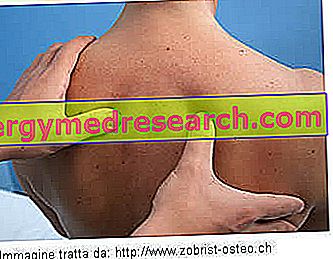
- Vasculitis can affect any type of blood vessel, resulting in a wide spectrum of diseases that can vary greatly in symptoms, severity and duration.
- The diagnosis can be confirmed by a biopsy of the tissue involved or by an angiography.
- The treatment is aimed at decreasing inflammation of the blood vessels and improving the function of the affected organs.
Diagnosis
Vasculitis is common to a heterogeneous group of diseases, each of which is defined by specific patterns of inflammation that are distinguished by:
- Type , size and location of the affected blood vessels;
- Cause and extent of the disease;
- Recognition of particular clinical anomalies;
- Possible involvement of tissues or organs.
The diagnosis of vasculitis is based on medical history, complete physical examination and results of laboratory tests.
Blood and urine tests
Blood tests are performed in case of active vasculitis. The results, in general, allow to highlight the signs of inflammation in the body, made evident by:
- High erythrocyte sedimentation rate (ESR);
- Increase in C-reactive protein (CRP);
- Anemia;
- Increased white blood cells (in particular, eosinophils);
- Increased platelet count.
Urinalysis can reveal abnormalities, such as the presence of hematuria and proteinuria (a sign of vasculitis affecting the kidneys). Other altered results may emerge from analyzes that assess the degree of involvement of different organs and their functionality.
Immunological test
Each type of vasculitis can produce a different clinical picture, but, in many cases, an immunological test can differentiate, confirm and monitor the presence of inflammation. These tests allow to detect high levels of cytoplasmic neutrophil antibodies (ANCA) and the formation of immune complexes (Kawasaki disease, Schonlein-Henoch purpura, etc.).
The three main ANCA-associated vasculitis are:
- Wegener's granulomatosis;
- Churg-Strauss syndrome;
- Microscopic polyangiitis.
Other forms, such as Behçet's disease and primary cerebral vasculitis, are not associated with alterations of specific hematochemical indices.
Diagnostic imaging
If the larger arteries, such as the aorta and its main branches, are affected, the doctor can show a decrease in blood flow through non-invasive imaging techniques (radiographs, computed tomography and magnetic resonance).
An angiography can show characteristic patterns of inflammation in the affected blood vessels. During the examination, a flexible and thin catheter is inserted into a large artery or vein and injects a contrast medium into the blood. The contours of the blood vessels are visible on the resulting radiographic images, allowing us to assess whether these are thickened, deformed, obstructed or restricted.
Bioptic diagnosis
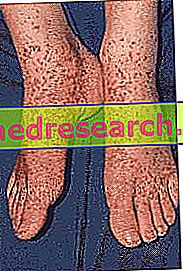
The definitive diagnosis of vasculitis is established after a biopsy of the affected blood vessel and of the tissue or organ involved (such as skin, kidney or lung). The biopsy survey allows the doctor to examine the small piece of tissue taken under the microscope to assess the presence of signs of inflammation.
Treatment
The treatment of the condition depends on the specific form of vasculitis, the areas / organs involved and the general health conditions of the patient. If the management of the disease is early, permanent damage can be avoided. Some types of vasculitis are self-limiting and can improve spontaneously, while others generally require drugs to stop inflammation and suppress the immune system.
Some measures may include:
- Steroids to control inflammation. The treatment for many types of vasculitis is the administration of a corticosteroid drug, such as prednisone or methylprednisolone, which helps reduce inflammation. The dose and duration of therapy depend on the extent and duration of the vasculitis. Side effects can be severe and long-term, especially if taken for a long period of time, they can include weight gain, diabetes and bone thinning (osteoporosis).
- Drugs for the control of the immune system. Cases of vasculitis that do not respond adequately to corticosteroids may require treatment with cytotoxic drugs. These work by suppressing the cells of the immune system, which are responsible for inflammation. Some examples include azathioprine and cyclophosphamide. New drugs designed to treat other autoimmune and inflammatory diseases can help dampen the immune system's response. Among these, rituximab has been approved for the treatment of granulomatosis and polyangiitis, cryoglobulinemic vasculitis and microscopic polyangiitis.
- Surgery . Affected organs (such as the heart or lungs) may require specific medical treatment designed to improve their function during the active phase of the disease. Damage caused by severe vasculitis sometimes requires surgery. This may involve, for example, a kidney transplant or grafting a vascular bypass to redirect blood flow.
In some cases, vasculitis can go into remission and recur at any time. Long-term drug treatment is often able to control the signs and symptoms of chronic forms. Rarely, vasculitis does not respond to therapy; this can lead to disability and even death of the patient.